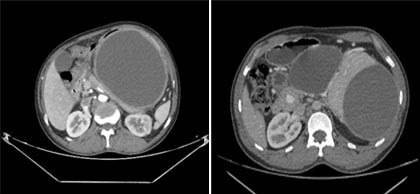
Impact of Fluid Collection According to Revised ATLANTA Classification on Patient Prognosis in Acute Pancreatitis: A Radiological Study
DOI:
https://doi.org/10.54133/ajms.v5i1S.258Keywords:
Acute pancreatitis, ATLANTA, Pseudocyst, Walled-off necrosisAbstract
Background: Acute pancreatitis is a complex and challenging disease. The revised Atlanta Classification emphasizes accurate characterization of collections that complicate acute pancreatitis and standardizes terminology across specialties, which helps to decide the treatment strategy. As a result, the role of imaging in the management of acute pancreatitis has substantially increased. Objective: This study aimed to categorize the fluid collections in acute pancreatitis using the 2012 ATLANTA classification and to compare the type of collection with the patient's clinical variables like length of hospital stay, ICU stay, presence of organ failure, type of organ failure, presence of infection, and outcome. Methods: This descriptive cross-sectional hospital-based study was conducted for two years. A total of 120 patients with acute pancreatitis-associated fluid collections were included in the study. Results: In our study, hospital and intensive care unit admission, as well as the length of stay, presence of organ failure, presence of infection, and the patient's outcome, all showed statistically significant relationships with walled-off necrosis (WON). Conclusions: The revised ATLANTA classification provides clear definitions to classify acute pancreatitis using easily identified clinical and radiologic criteria and thereby helps to determine the proper patient outcome and management.
Downloads
References
Fawzy HA, Mohammed AA, Fawzy HM, Fikry EM. Reorienting of pramipexole as a promising therapy for acute pancreatitis in a rat model by suppressing TLR4NF-κB p65NLRP3 inflammasome signaling. Can J Physiol Pharmacol. 2022;100(6):542-552. doi: 10.1139/cjpp-2021-0664. DOI: https://doi.org/10.1139/cjpp-2021-0664
Busireddy KK, AlObaidy M, Ramalho M, Kalubowila J, Baodong L, Santagostino I, Semelka RC. Pancreatitis-imaging approach. World J Gastrointest Pathophysiol. 2014;5(3):252-70. doi: 10.4291/wjgp.v5.i3.252. DOI: https://doi.org/10.4291/wjgp.v5.i3.252
Banday IA, Gattoo I, Khan AM, Javeed J, Gupta G, Latief M. Modified Computed Tomography Severity Index for Evaluation of Acute Pancreatitis and its Correlation with Clinical Outcome: A Tertiary Care Hospital Based Observational Study. J Clin Diagn Res. 2015;9(8):TC01-5. doi: 10.7860/JCDR/2015/14824.6368. DOI: https://doi.org/10.7860/JCDR/2015/14824.6368
Thoeni RF. The revised Atlanta classification of acute pancreatitis: its importance for the radiologist and its effect on treatment. Radiology. 2012;262(3):751-64. doi: 10.1148/radiol.11110947. DOI: https://doi.org/10.1148/radiol.11110947
García AH, Calderón AV, López RA, Pérez JL, Mendoza AC. Endoscópic Peri Pancreatic Fluid Collection Drainage Guided by USE in a Highly Complex Hospital in Lima, Peru. A First National Case Series. Gastroenterol Hepatol Open Access. 2017;6(1):00183. DOI: 10.15406/ghoa.2017.06.00183 DOI: https://doi.org/10.15406/ghoa.2017.06.00183
Komara NL, Paragomi P, Greer PJ, Wilson AS, Breze C, Papachristou GI, Whitcomb DC. Severe acute pancreatitis: capillary permeability model linking systemic inflammation to multiorgan failure. Am J Physiol Gastrointest Liver Physiol. 2020;319(5):G573-G583. doi: 10.1152/ajpgi.00285.2020. DOI: https://doi.org/10.1152/ajpgi.00285.2020
Walkowska J, Zielinska N, Tubbs RS, Podgórski M, Dłubek-Ruxer J, Olewnik Ł. Diagnosis and Treatment of Acute Pancreatitis. Diagnostics (Basel). 2022;12(8):1974. doi: 10.3390/diagnostics12081974. DOI: https://doi.org/10.3390/diagnostics12081974
Forsmark CE, Baillie J; AGA Institute Clinical Practice and Economics Committee; AGA Institute Governing Board. AGA Institute technical review on acute pancreatitis. Gastroenterology. 2007;132(5):2022-44. doi: 10.1053/j.gastro.2007.03.065. DOI: https://doi.org/10.1053/j.gastro.2007.03.065
Büchler MW, Gloor B, Müller CA, Friess H, Seiler CA, Uhl W. Acute necrotizing pancreatitis: treatment strategy according to the status of infection. Ann Surg. 2000;232(5):619-26. doi: 10.1097/00000658-200011000-00001. DOI: https://doi.org/10.1097/00000658-200011000-00001
Bezmarević M, van Dijk SM, Voermans RP, van Santvoort HC, Besselink MG. Management of (Peri)Pancreatic Collections in Acute Pancreatitis. Visc Med. 2019;35(2):91-96. doi: 10.1159/000499631. DOI: https://doi.org/10.1159/000499631
Alkareemy EAR, Ahmed LA, El-Masry MA, Habib HA, Mustafa MH. Etiology, clinical characteristics, and outcomes of acute pancreatitis in patients at Assiut University Hospital. The Egyptian Journal of Internal Medicine. 2020;32:1-6. https://doi.org/10.1186/s43162-020-00025-w. DOI: https://doi.org/10.1186/s43162-020-00025-w
Shafiq F, Khan MF, Asghar MA, Shamim F, Sohaib M. Outcome of patients with acute pancreatitis requiring intensive care admission: A retrospective study from a tertiary care center of Pakistan. Pak J Med Sci. 2018;34(5):1082-1087. doi: 10.12669/pjms.345.15575. DOI: https://doi.org/10.12669/pjms.345.15575
Lankisch PG, Pflichthofer D, Lehnick D. No strict correlation between necrosis and organ failure in acute pancreatitis. Pancreas. 2000;20(3):319-22. doi: 10.1097/00006676-200004000-00015 DOI: https://doi.org/10.1097/00006676-200004000-00015
Shaheen MA, Akhtar AJ. Organ failure associated with acute pancreatitis in African-American and Hispanic patients. Journal of the National Medical Association. 2007;99(12):1402-6.
Petrov MS, Shanbhag S, Chakraborty M, Phillips AR, Windsor JA. Organ failure and infection of pancreatic necrosis as determinants of mortality in patients with acute pancreatitis. Gastroenterology. 2010;139(3):813-20. doi: 10.1053/j.gastro.2010.06.010. DOI: https://doi.org/10.1053/j.gastro.2010.06.010
Fu CY, Yeh CN, Hsu JT, Jan YY, Hwang TL. Timing of mortality in severe acute pancreatitis: experience from 643 patients. World J Gastroenterol. 2007;13(13):1966-9. doi: 10.3748/wjg.v13.i13.1966. DOI: https://doi.org/10.3748/wjg.v13.i13.1966
Balthazar EJ, Fisher LA. Hemorrhagic complications of pancreatitis: radiologic evaluation with emphasis on CT imaging. Pancreatology. 2001;1(4):306-13. doi: 10.1159/000055829. DOI: https://doi.org/10.1159/000055829
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Al-Rafidain Journal of Medical Sciences ( ISSN 2789-3219 )

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Published by Al-Rafidain University College. This is an open access journal issued under the CC BY-NC-SA 4.0 license (https://creativecommons.org/licenses/by-nc-sa/4.0/).