The Relationship Between OqxAB Efflux Pump and Drug Resistance in Klebsiella pneumoniae Isolated from Clinical Sources
DOI:
https://doi.org/10.54133/ajms.v5i1S.309Keywords:
Antibiotic resistance, Efflux pump, Klebsiella spp., OqxAB geneAbstract
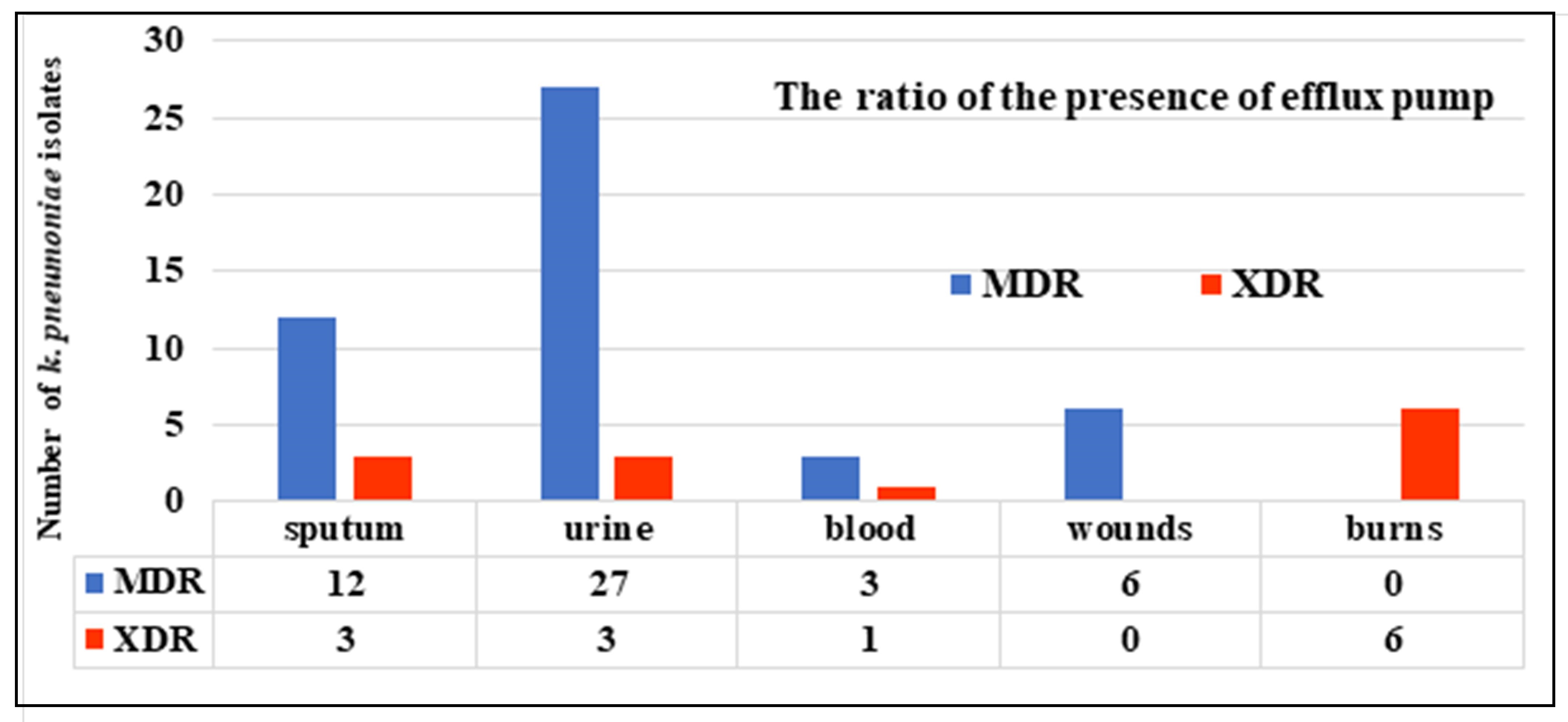
Background: Because Klebsiella pneumoniae resistance to the majority of antibiotics is developing quickly, it is important to study the efflux pump system that bacteria carry and the genes that encode them in order to find effective ways to stop or limit this resistance. Objective: To find out how common OqxAB-efflux pump genes are and if there is a link between these genes and antibiotic resistance in Klebsiella pneumoniae that has been isolated from different clinical sources. Method: In this investigation, 174 various clinical specimens were collected from Baghdad hospitals. Based on morphological characteristics, culture media, biochemical testing, the Vitek-2 system, and molecular diagnosis by the 16S rRNA gene, only 97 isolates were recognized as Klebsiella pneumoniae. The antibiotic susceptibility of the isolates to 21 antibiotics was also determined. The presence of the active efflux pump was determined phenotypically (ethidium-bromide cartwheel method) and genotypically by multiplex PCR. Results: All isolates were resistant to ampicillin and amoxicillin-clavulanate (100%). On the other hand, the percentage of resistance to cefotaxime, ceftazidime, and cefixime was 95.87%, 94.84%, and 95.87%, respectively. While tigecycline had the lowest resistance rate (11.43%), In the genotype detection assay for efflux pump genes, the results show that the percentages of oqx A and oqx B are 65% and 83.6%, respectively. Conclusion: The oqxA and oqxB genes have a direct relationship with antibiotic resistance in Klebsiella pneumoniae.
Downloads
References
Onori R, Gaiarsa S, Comandatore F, Pongolini S, Brisse S, Colombo A, et al. Tracking nosocomial Klebsiella pneumoniae infections and outbreaks by whole-genome analysis: small-scale Italian scenario within a single hospital. J Clin Microbiol. 2015;53(9):2861-2868. doi: 10.1128/JCM.00545-15.
Paczosa MK, Mecsas J. Klebsiella pneumoniae: going on the offense with a strong defense. Microbiol Mol Biol Rev. 2016;80(3):629-661. doi: 10.1128/MMBR.00078-15.
Ni RT, Onishi M, Mizusawa M, Kitagawa R, Kishino T, Matsubara F, et al. The role of RND-type efflux pumps in multidrug-resistant mutants of Klebsiella pneumoniae. Sci Rep. 2020;10(1):10876. doi; 10.1038/s41598-020-67820-x.
Carvalho I, Chenouf NS, Carvalho JA, Castro AP, Silva V, Capita R, et al. Multidrug-resistant Klebsiella pneumoniae harboring extended spectrum β-lactamase encoding genes isolated from human septicemias. PLoS One. 2021;4;16(5):e0250525. doi: 10.1371/journal.pone.0250525.
Veleba M, Higgins PG, Gonzalez G, Seifert H, Schneiders T. Characterization of RarA, a novel AraC family multidrug resistance regulator in Klebsiella pneumoniae. Antimicrob Agent Chemother. 2012;56(8):4450-4458. doi: 10.1128/aac.00456-12.
Szabo O, Kocsis B, Szabo N, Kristof K, Szabo D. Contribution of OqxAB efflux pump in selection of fluoroquinolone-resistant Klebsiella pneumoniae. Can J Infect Dis Med Microbiol. 2018;1;2018. doi: 10.1155/2018/4271638.
Hansen LH, Jensen LB, Sørensen HI, Sørensen SJ. Substrate specificity of the OqxAB multidrug resistance pump in Escherichia coli and selected enteric bacteria. J Antimicrob Chemother. 2007;1;60(1):145-147. doi: 10.1093/jac/dkm167.
Bharatham N, Bhowmik P, Aoki M, Okada U, Sharma S, Yamashita E, et al. Structure and function relationship of OqxB efflux pump from Klebsiella pneumoniae. Nature Commun. 2021;13;12(1):5400. doi: 10.1038/s41467-021-25679-0.
Li XZ, Plésiat P, Nikaido H. The challenge of efflux-mediated antibiotic resistance in Gram-negative bacteria. Clin Microbiol Rev. 2015;28(2):337-418. doi: 10.1128/cmr.00117-14.
CLSI, 2022. Performance Standards for Antimicrobial Susceptibility Testing, (32nd ed.), CLSI supplement M100. Clinical and Laboratory Standards Institute: 32-34.
US Food and Drug Administration. FDA-Identified Interpretive Criteria for Tigecycline-Injection products; 2019.
Martins M, McCusker MP, Viveiros M, Couto I, Fanning S, Pagès J, et al. Simple method for assessment of MDR bacteria for over-expressed efflux pumps. Open Microbiol J. 2013;7:72. doi: 10.2174/1874285801307010072.
Cary N. Statistical analysis system, User's guide. Statistical. Version 9. SAS. Inst. Inc. USA. 2012.
Ghaima TM. Molecular detection of acrAB and oqxAB genes in Klebsiella pneumoniae and evaluation the effect of berberine on their gene expression. Iraqi J Biotechnol. 2022;21(2):124-135.
Seifi K, Kazemian H, Heidari H, Rezagholizadeh F, Saee Y, Shirvani F, et al. Evaluation of biofilm formation among Klebsiella pneumoniae isolates and molecular characterization by ERIC-PCR. Jundishapur J Microbiol. 2016;9(1). doi: 10.5812/jjm.30682.
Amani I, Salehi MB, Mansour FN. Frequency of prevalence of Klebsiella pneumoniae in clinical samples and the evaluation of the role of efflux pump in determining antibiotic resistance. Khazar J Sci Technol. 2020;4(1):41-64. doi: 10.5782/2520-6133.2020.4.1.41.
Magiorakos AP, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;1;18(3):268-281. doi: 10.1111/j.1469-0691.2011.03570.x.
Gawad WE, Helmy OM, Tawakkol WM, Hashem AM. Antimicrobial resistance, biofilm formation, and phylogenetic grouping of uropathogenic Escherichia coli isolates in Egypt: The role of efflux pump-mediated resistance. Jundishapur J Microbiol. 2018;11(2). doi: 10.5812/jjm.14444.
Rana T, Kaur N, Farooq U, Khan A, Singh S. Efflux as an arising cause of drug resistance in Punjab-India. IJBPAS, 2015;4(9):5967-5979.
Akinpelu S, Ajayi A, Smith SI, Adeleye AI. Efflux pump activity, biofilm formation and antibiotic resistance profile of Klebsiella spp. isolated from clinical samples at Lagos University Teaching Hospital. BMC Res Notes. 2020;13:1-5. doi:10.1186/s13104-020-05105-2.
Li J, Zhang H, Ning J, Sajid A, Cheng G, Yuan Z, et al. The nature and epidemiology of OqxAB, a multidrug efflux pump. Antimicrob Resist Infect Control. 2019;8(1):1-3. doi: 10.1186/s13756-019-0489-3.
Dehnamaki M, Ghane M, Babaeekhou L. Detection of OqxAB and QepA efflux pumps and their association with antibiotic resistance in Klebsiella pneumoniae isolated from urinary tract infection. Int J Infect. 2020;31;7(4). doi: 10.5812/iji.107397.
Amereh F, Arabestani MR, Shokoohizadeh L. Relationship of OqxAB efflux pump to antibiotic resistance, mainly fluoroquinolones in Klebsiella pneumoniae, isolated from hospitalized patients. Iranian J Basic Med Sci. 2023;26(1):93. doi: 10.22038/IJBMS.2022.67095.14714.
Xu Q, Jiang J, Zhu Z, Xu T, Sheng ZK, Ye M, et al. Efflux pumps AcrAB and OqxAB contribute to nitrofurantoin resistance in an uropathogenic Klebsiella pneumoniae isolate. Int J Antimicrob Agent. 2019;1;54(2):223-227. doi: 10.1016/j.ijantimicag.2019.06.004.
Ho PL, Ng KY, Lo WU, Law PY, Lai EL, Wang Y, et al. Plasmid-mediated OqxAB is an important mechanism for nitrofurantoin resistance in Escherichia coli. Antimicrob Agent Chemother. 2016;60(1):537-543. doi: 10.1128/aac.02156-15.
Wyres KL, Holt KE. Klebsiella pneumoniae as a key trafficker of drug resistance genes from environmental to clinically important bacteria. Curr Opin Microbiol. 2018;1;45:131-139. doi: 10.1016/j.mib.2018.04.004.
Razavi S, Mirnejad R, Babapour E. Involvement of AcrAB and OqxAB efflux pumps in antimicrobial resistance of clinical isolates of Klebsiella pneumonia. J Appl Biotechnol Rep. 2020;1;7(4):251. doi: 7.10.30491/JABR.2020.120179.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Al-Rafidain Journal of Medical Sciences ( ISSN 2789-3219 )

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Published by Al-Rafidain University College. This is an open access journal issued under the CC BY-NC-SA 4.0 license (https://creativecommons.org/licenses/by-nc-sa/4.0/).