Preparation and Effects of Manganese Oxide Nanoparticles Against Quinolone-Resistant Bacteria Isolated from Hospital Wastewater
DOI:
https://doi.org/10.54133/ajms.v6i2.728Keywords:
Antibacterial activity, Antibiofilm effect, Bacterial resistance, MnO2NPsAbstract
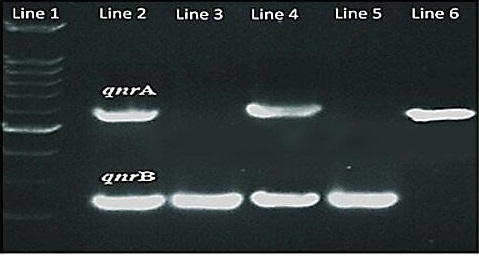
Background: The widespread administration of quinolones may have led to an increase in bacterial resistance development. Objective: To synthesize and characterize manganese oxide nanoparticles (MnO2NPs) and evaluate their effects on the viability and biofilm formation of quinolone-resistant gram-positive and negative pathogenic bacteria. Methods: We prepared MnO2NPs using the photo-irradiation method and recorded their characteristics using XRD, TEM, and SEM. Staphylococcus aureus, Streptococcus pneumonia, Escherichia coli, Klebsiella pneumonia, and Pseudomonas aeruginosa were collected from the wastewater of Baghdad hospitals during the period from July 3rd to July 14th, 2023. We used the VITEK2 system to confirm and identify all of the isolates. We conducted biofilm formation and antibiotic susceptibility tests using nalidixic acid, ciprofloxacin, norfloxacin, aztreonam, levofloxacin, and ofloxacin, and also detected the qnrA and qnrB genes. Finally, we evaluated the effects of the prepared nanoparticles on the viability and biofilm formation of bacterial isolates. Results: MnO2NPs characterizations showed a diffraction peak at 2θ values with 21 nm average sizes; qnrA and qnrB genes were found in three and four isolates, respectively; and significant effects of MnO2NPs against viability and biofilm formation were recorded. Conclusions: The synthesized nanoparticles have antibacterial and anti-biofilm activities against a variety of bacteria possessing qnr genes. Even multi-resistant bacterial isolates have the potential to be strong antimicrobial agents against these pathogens.
Downloads
References
AboKsour MF, Al-Jubori SS, Jawad HA. Influence of Helium-Neon laser on some virulence factors of Staphylococcus aureus and Escherichia coli. Al-Mustansiriyah J Sci. 2018;9(3):29. doi: 10.23851/mjs.v29i3.619.
Zeng W, Xu W, Xu Y, Liao W, Zhao Y, Zheng X, et al. The prevalence and mechanism of triclosan resistance in Escherichia coli isolated from urine samples in Wenzhou, China. Antimicrob Resist Infect Control. 2020;9(1):161. doi: 10.1186/s13756-020-00823-5.
Atmanto Y, Adi K, Abd Kadir N, Rusli B. Extended spectrum beta lactamase (ESBL) confirmation test using E-Test. Int J Recent Adv Multidiscipl Topics. 2022:5;125-130.
Adarsha JR, Ravishankar TN, Ananda A, Manjunatha CR, Shilpa BM, Ramakrishnappa T. Hydrothermal synthesis of novel heterostructured Ag/TiO2 /CuFe2O4 nanocomposite: Characterization, enhanced photocatalytic degradation of methylene blue dye, and efficient antibacterial studies. Water Environ Res. 2022;94(6):e10744. doi: 10.1002/wer.10744.
Chen SC, Kuo TY, Lin HC, Chen RZ, Sun H. Optoelectronic properties of p-type NiO films deposited by direct current magnetron sputtering versus high power impulse magnetron sputtering. Appl Surf Sci. 2020;50(8):14-19. doi:10.1016/j.apsusc.2019.145106.
Flemming H, Wingender J, Szewzyk U, Steinberg P, Rice S A, Kjelleberg S. Biofilms: an emergent form of bacterial life. Nat. Rev. Microbio. 2016;9(14):563–575. doi: 10.1038/nrmicro.2016.94.
Mohamed K, Zine K, Fahima K, Abdelfattah E, Sharifudin SM, Duduku K. NiO nanoparticles induce cytotoxicity mediated through ROS generation and impairing the antioxidant defence in the human lung epithelial cells (A549): Preventive of Pistacia lentiscus essential oil. Toxicol Rep. 2018:5;480–488. doi: 10.1016/j.toxrep.2018.03.012.
da Silva B, Paiva Abuçafy M, Manaia B, Junior J, Chiari-Andréo B, Pietro R, et al. Relationship between structure and antimicrobial activity of zinc oxide nanoparticles: An overview. Int J Nanomed. 2019:14; 9395–9410. doi: 10.2147/IJN.S216204.
Ramalingam V, Sundaramahalingam S, Rajaram R. Size-dependent antimycobacterial activity of titanium oxide nanoparticles against Mycobacterium tuberculosis. J Mater Chem. 2019;7:4338–4346. doi: 10.1039/C9TB00784A.
Kannan K, Radhika D, Sadasivuni KK, Reddy KR, Raghu AV. Nanostructured metal oxides and its hybrids for photocatalyticand biomedical applications. Adv Col Int Sci. 2020;281:102178. doi: 10.1016/j.cis.2020.102178.
Shkir M, Yahia IS, Ganesh V, Bitla Y, Ashraf IM, Kaushik A, et al. A facile synthesis of Au-nanoparticles decorated PbI2 single crystalline nanosheets for optoelectronic device applications. Sci Rep. 2018;8(7):13806. doi: 10.1038/s41598-018-32038-5.
Rheima AM, Al Marjani MF, Aboksour MF, Hashim SM. Evaluation of anti-biofilm formation effect of nickel oxide nanoparticles (NiO-NPs) against methicillin-resistant Staphylococcus aureus (MRSA). Int J of Nanosci Nanotechnol. 2021;17(4):221-230. doi: ijnnonline.net/article_247640.html.
Mohammed FA. Presence of extended-spectrum β-Lactamases genes in E. coli isolated from farm workers in the South of London. IJPQA 2018;9(1):64-67 doi: 10.25258/ijpqa.v9i01.11361.
Humphries R, Bobenchik AM, Hindler JA, Schuetz AN. Overview of changes to the clinical and laboratory standards institute performance standards for antimicrobial susceptibility testing. J Clin Microbiol. 2021;59(12):e0021321. doi:10.1128/jcm.00213-21.
Sirelkhatim A, Mahmud S, Seeni A, Kaus NHM, Ann LC, Bakhori SKM, et al. Review on zinc oxide nanoparticles: Antibacterial activity and toxicity mechanism. Nanomicro Lett. 2015;7(3):219-242. doi: 10.1007/s40820-015-0040-x.
Rodríguez JM, Cano ME, Velasco C, Martínez L, Pascual Á. Plasmid-mediated quinolone resistance: an update. J Infect Chemother. 2021;17(2):149-182. doi: 10.1007/s10156-010-0120-2.
Saki M, Farajzadeh Sheikh A, Seyed-Mohammadi S, Asareh Zadegan Dezfuli A, Shahin M, Tabasi M, et al. Occurrence of plasmid-mediated quinolone resistance genes in Pseudomonas aeruginosa strains isolated from clinical specimens in southwest Iran: a multicentral study. Sci Rep. 2022;12(1):2296. doi: 10.1038/s41598-022-06128-4.
Nsofor CM, Tattfeng MY, Nsofor CA. High prevalence of qnrA and qnrB genes among fluoroquinolone-resistant Escherichia coli isolates from a tertiary hospital in Southern Nigeria. Bull Natl Res Cent. 2021;45(26):2-7. doi: 10.1186/s42269-020-00475-w.
Esmaeel NE, Gerges MA, Hosny TA, Ali AR, Gebriel MG. Detection of chromosomal and plasmid-mediated quinolone resistance among Escherichia coli isolated from urinary tract infection cases; Zagazig University Hospitals, Egypt. Infe Dru Resist. 2020:13;413–421. doi: 10.2147/IDR.S240013.
Mayers DL, Lerner SA, Ouelette M. Antimicrobial drug resistance C: Clinical and Epidemiological Aspects; Sprin Dor Heid. 2019;681–1347. doi: 10.1007/978-1-60327-595-8.
Martin I, Sawatzky P, Liu G. Antimicrobial resistance to Neisseria gonorrhoeae in Canada: 2009–2013. Can Commun Dis Rep. 2015: 41(2):35-41. doi: 10.14745/ccdr.v41i02a04.
Mabona U, Viljoen A, Shikanga E. Antimicrobial activity of Southern African medicinal plants with dermatological relevance: from an ethno pharmacological screening approach, to combination studies and the isolation of a bioactive compound. J Ethnopharmacol. 2013;148(1):45–55. doi: 10.1016/j.jep.2013.03.056.
Fahs A, Quiles F, Jamal D, Humbert F, Francius G. In situ analysis of bacterial extracellular polymeric substances from a Pseudomonas fluorescens biofilm by combined vibrational and single molecule force spectroscopies. J Phys Chem. 2014;118(24):6702-6713. doi: 10.1021/jp5030872.
Rabiei M, Palevicius A, Monshi A, Nasiri S, Vilkauskas A, Janusas G. Comparing methods for calculating nano crystal size of natural hydroxyapatite using X-ray diffraction. Nanomaterials. 2020;10(9):1627. doi: 10.3390/nano10091627.
Altammar KA. A review on nanoparticles: characteristics, synthesis, applications, and challenges. Fron Microbiol. 2023;17(14):115-126. doi: 10.3389/fmicb.2023.1155622.
Islam F, Shohag S, Uddin MJ, Islam MR, Nafady MH, Akter A, et al. Exploring the journey of zinc oxide nanoparticles (ZnO-NPs) toward biomedical applications. Materials. 2022;15(6):2160. doi: 10.3390/ma15062160.
Khan I, Saeed K, Khan I. Nanoparticles: Properties, applications and toxicities. Arab J Chem. 2019;12(7): 908–931. doi: 10.1016/j.arabjc.2017.05.011.
Kučuk N, Primožič M, Knez Ž, Leitgeb M. Sustainable biodegradable biopolymer-based nanoparticles for healthcare applications. Int J Mol Sci. 2023;24(4):3188. doi: 10.3390/ijms24043188.
Abid H, Mohd J, Ravi PS, Shanay R, Rajiv S. Applications of nanotechnology in medical field: a brief review. Glob Health J. 2023;7(2):70-77. doi: 10.1016/j.glohj.2023.02.008.
AboKsour MF, Shafiq SA, Mussa AH. An Evaluation of water pollution in the Southern Iraqi marshes by using bacterial indicators and other related parameters. J Glog Pharm Technol. 2017;10(9):412-418.
Zhao YC, Sun ZH, Xiao MX, Li JK, Liu HY, et al. Analysing the correlation between quinolone-resistant Escherichia coli resistance rates and climate factors: A comprehensive analysis across 31 Chinese provinces. Environ Res. 2024;245:117995. doi: 10.1016/j.envres.2023.117995.
Murray BO, Flores C, Williams C, Flusberg DA, Marr EE, Kwiatkowska KM, et al. Recurrent urinary tract infection: a mystery in search of better model systems. Fron Cell Infect Microbiol. 2021;11:691210. doi: 10.3389/fcimb.2021.691210.
Qamar U, Aatika M. Impact of climate change on antimicrobial resistance dynamics: an emerging One Health challenge. Future Microbiol. 2023;18:535-539. doi:10.2217/fmb-2023-0022.
Du T, Chen S, Zhang J, Li T, Li P, Liu J, et al. Antibacterial activity of manganese dioxide nanosheets by ROS-mediated pathways and destroying membrane integrity. Nanomaterials (Basel). 2020;10(8):1545-58. doi: 10.3390/nano10081545.
Zaki A, Siddiqui MR, Khan SA. Use of manganese oxide nanoparticle (MnO2NPs) and Pseudomonas putida for the management of wilt disease complex of carrot. Experimental Parasitology. Exp Parasitol. 2024;257:108698. doi: 10.1016/j.exppara.2024.108698.
Peymani A, Farivar TN, Najafipour R, Mansouri S. High prevalence of plasmid-mediated quinolone resistance determinants in Enterobacter cloacae isolated from hospitals of the Qazvin, Alborz, and Tehran provinces, Iran. Rev Soc Bras Med Trop. 2016;49(3):286–291. doi: 10.1590/0037-8682-0454-2015.
Tageldin M, Babier AM, Elhasan OA, Yousif M, Ahemir SY, Hussien, HM. et al. Molecular Detection of Plasmid-Mediated Quinolone Resistance Genes (qnrA and aac(6′)-Ib-cr) in Drug Resistant Escherichia coli, Sudan. Microb Res J Int. 2023;33(4):14-21. doi: 10.9734/mrji/2023/v33i41375.
Song Z, Wu Y, Wang H, Han H. Synergistic antibacterial effects of curcumin modified silver nanoparticles through ROS-mediated pathways. Mater Sci Eng C Mater Biol Appl. 2019;99:255-263. doi: 10.1016/j.msec.2018.12.053.
Zheng H, Ji Z, Roy KR, Gao M, Li R. Engineered graphene oxide nanocomposite capable of preventing the evolution of antimicrobial resistance. ACS Nano. 2019:13:11488–11499. doi: 10.1021/acsnano.9b04970.
Fan W, Bu W, Shen B, He Q, Cui Z, Liu Y, et al. Intelligent MnO2 nanosheets anchored with upconversion nanoprobes for concurrent pH-/H2O2 -responsive UCL imaging and oxygen-elevated synergetic therapy. Adv Mater. 2022:27;4155–4161. doi: 10.1002/adma.201405141.
Yang Q, Wang X, Peng H, Arabi M, Li J, Xiong H, et al. Ratiometric fluorescence and colorimetry dual-mode assay based on manganese dioxide nanosheets for visual detection of alkaline phosphatase activity. Sens. Actuat. B Chem. 2020:302:127176. doi: 10.1016/j.snb.2019.127176.
Chen SC, Kuo TY, Lin HC, Chen R Z, Sun H. Optoelectronic properties of p-type NiO films deposited by direct current magnetron sputtering versus high power impulse magnetron sputtering. Appl Surf Sci. 2020:508, 145106. doi:10.1016/j.apsusc.2019.145106.
Song Z, Wu Y, Wang H, Han H. Synergistic antibacterial effects of crcumin modified silver nanoparticles through ROS-mediated pathways. Mater Sci Eng C Mater Biol Appl. 2019;99:255-263. doi: 10.1016/j.msec.2018.12.053.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Al-Rafidain Journal of Medical Sciences ( ISSN 2789-3219 )

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Published by Al-Rafidain University College. This is an open access journal issued under the CC BY-NC-SA 4.0 license (https://creativecommons.org/licenses/by-nc-sa/4.0/).