Preoperative Leg Pain as a Predictor of Clinical Outcomes after Single Lumbar Microdecompression Surgery in Young and Middle-Aged Groups: A Retrospective Study
DOI:
https://doi.org/10.54133/ajms.v6i2.737Keywords:
Clinical outcome, Leg pain, Microdecompression, Microdiscectomy, Predictors, RadiculopathyAbstract
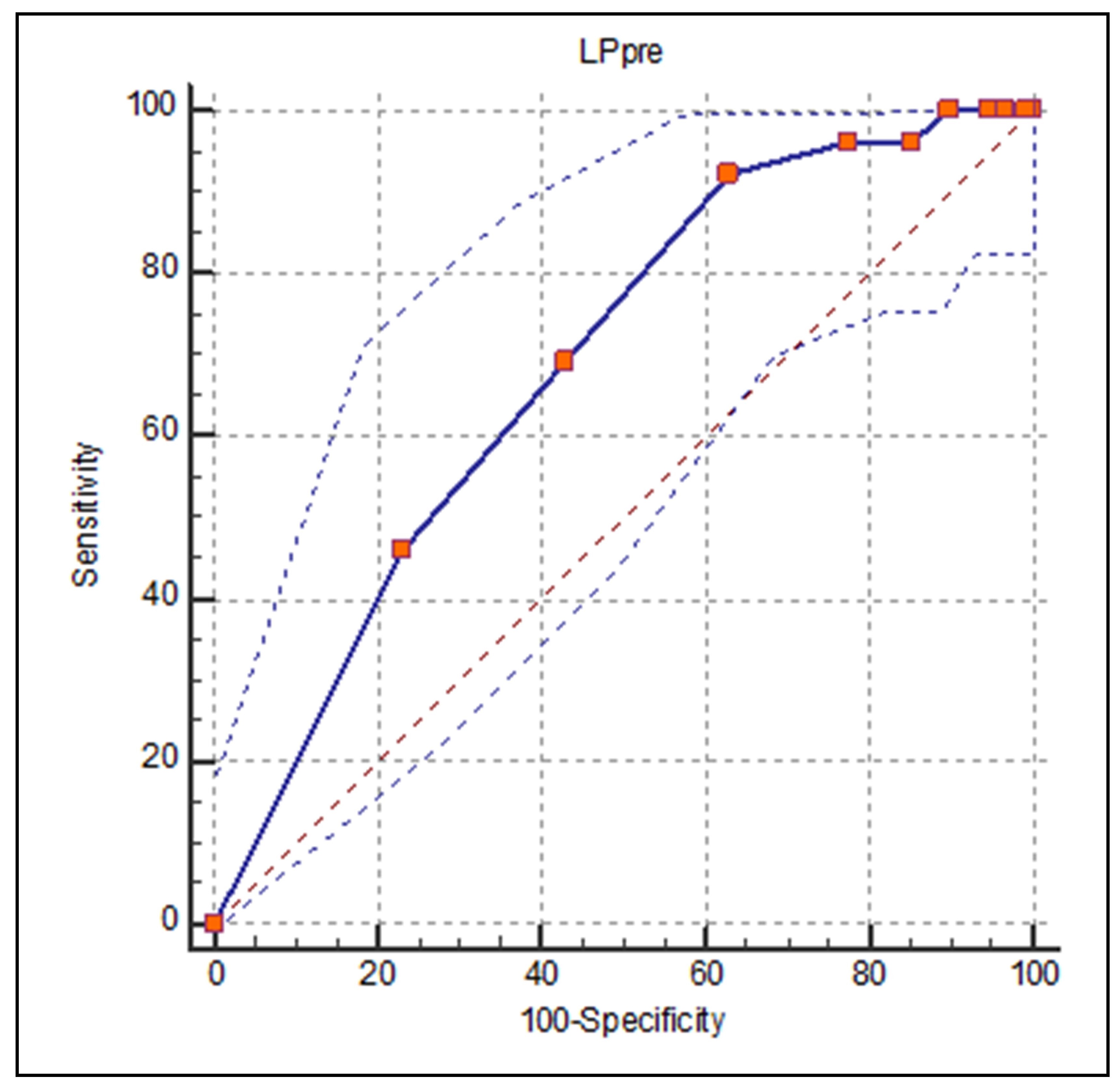
Background: Previous studies have stated that the higher the LP VAS, the better the outcome. However, there is no quantification of this relationship. Objectives: To maximize the understanding of the effect of symptom duration and intensity of leg pain on surgical outcome at one year, ascertain whether the level of radiculopathy influences outcome, and examine the possible factors that may lead to repeat surgery at the same level in young and middle age groups. Methods: Retrospective data was collected from patients who underwent primary, single-level lumbar decompression surgery with a 12-month follow-up period. We used the ROC curve to determine the LP VAS cutoff value. Results: 500 patients were included. There was a significant improvement in LBP VAS and LP VAS after 12-month follow-up (84% and 95%, respectively). There was a significant relationship between the reoperation rate and LP VAS, with a p-value of 0.001. LP VAS (>7.0) is the maximum area under the curve, with 92% sensitivity and 37% specificity to predict reoperation. There was no significant relationship with the duration of radiculopathy. Conclusions: Patients (92%) with a preoperative LP VAS >7.0 are more susceptible to re-operation surgery. LP cannot be used as a predictor of surgical outcome independently of other factors. Surgeons should be more cautious in selecting patients for surgery and not base their decision only on preoperative leg pain.
Downloads
References
Pearson AM, Blood EA, Frymoyer JW, Herkowitz H, Abdu WA, Woodward R, et al. SPORT lumbar intervertebral disk herniation and back pain: does treatment, location, or morphology matter? Spine (Phila Pa 1976). 2008;33(4):428-435. doi: 10.1097/BRS.0b013e31816469de.
Awad JN, Moskovich R. Lumbar disc herniations: surgical versus nonsurgical treatment. Clin Orthop Relat Res. 2006;443:183-197. doi: 10.1097/01.blo.0000198724.54891.3a.
Haugen AJ, Brox JI, Grøvle L, Keller A, Natvig B, Soldal D, et al. Prognostic factors for non-success in patients with sciatica and disc herniation. BMC Musculoskelet Disord. 2012;13:183. doi: 10.1186/1471-2474-13-183.
Huang W, Han Z, Liu J, Yu L, Yu X. Risk factors for recurrent lumbar disc herniation: A systematic review and meta-analysis. Medicine (Baltimore). 2016;95(2):e2378. doi: 10.1097/MD.0000000000002378.
Spratt KF, Keller TS, Szpalski M, Vandeputte K, Gunzburg R. A predictive model for outcome after conservative decompression surgery for lumbar spinal stenosis. Eur Spine J. 2004;13(1):14-21. doi: 10.1007/s00586-003-0583-2.
Hebert JJ, Fritz JM, Koppenhaver SL, Thackeray A, Kjaer P. Predictors of clinical outcome following lumbar disc surgery: the value of historical, physical examination, and muscle function variables. Eur Spine J. 2016;25(1):310-317. doi: 10.1007/s00586-015-3916-z.
Parker SL, Mendenhall SK, Godil SS, Sivasubramanian P, Cahill K, Ziewacz J, et al. Incidence of low back pain after lumbar discectomy for herniated disc and its effect on patient-reported outcomes. Clin Orthop Relat Res. 2015;473(6):1988-1999. doi: 10.1007/s11999-015-4193-1.
Silverplats K, Lind B, Zoega B, Halldin K, Rutberg L, Gellerstedt M, et al. Clinical factors of importance for outcome after lumbar disc herniation surgery: long-term follow-up. Eur Spine J. 2010;19(9):1459-1467. doi: 10.1007/s00586-010-1433-7.
Cook CE, Arnold PM, Passias PG, Frempong-Boadu AK, Radcliff K, Isaacs R. Predictors of pain and disability outcomes in one thousand, one hundred and eight patients who underwent lumbar discectomy surgery. Int Orthop. 2015;39(11):2143-2151. doi: 10.1007/s00264-015-2748-0.
Wilson CA, Roffey DM, Chow D, Alkherayf F, Wai EK. A systematic review of preoperative predictors for postoperative clinical outcomes following lumbar discectomy. Spine J. 2016;16(11):1413-1422. doi: 10.1016/j.spinee.2016.08.003.
den Boer JJ, Oostendorp RA, Beems T, Munneke M, Oerlemans M, Evers AW. A systematic review of bio-psychosocial risk factors for an unfavourable outcome after lumbar disc surgery. Eur Spine J. 2006;15(5):527-536. doi: 10.1007/s00586-005-0910-x.
Abdu RW, Abdu WA, Pearson AM, Zhao W, Lurie JD, Weinstein JN. Reoperation for recurrent intervertebral disc herniation in the spine patient outcomes research trial: Analysis of rate, risk factors, and outcome. Spine (Phila Pa 1976). 2017 ;42(14):1106-1114. doi: 10.1097/BRS.0000000000002088.
Lee BH, Yang JH, Lee HM, Park JY, Park SE, Moon SH. Surgical outcome predictor in degenerative lumbar spinal disease based on health related quality of life using Euro-Quality 5 Dimensions Analysis. Yonsei Med J. 2016;57(5):1214-1221. doi: 10.3349/ymj.2016.57.5.1214.
Sedighi M, Haghnegahdar A. Lumbar disk herniation surgery: outcome and predictors. Global Spine J. 2014;4(4):233-244. doi: 10.1055/s-0034-1390010.
Dewing CB, Provencher MT, Riffenburgh RH, Kerr S, Manos RE. The outcomes of lumbar microdiscectomy in a young, active population: correlation by herniation type and level. Spine (Phila Pa 1976). 2008;33(1):33-38. doi: 10.1097/BRS.0b013e31815e3a42.
Kleinstück FS, Grob D, Lattig F, Bartanusz V, Porchet F, Jeszenszky D, et al. The influence of preoperative back pain on the outcome of lumbar decompression surgery. Spine (Phila Pa 1976). 2009;34(11):1198-1203. doi: 10.1097/BRS.0b013e31819fcf35.
Kleinstueck FS, Fekete T, Jeszenszky D, Mannion AF, Grob D, Lattig F, et al. The outcome of decompression surgery for lumbar herniated disc is influenced by the level of concomitant preoperative low back pain. Eur Spine J. 2011;20(7):1166-1173. doi: 10.1007/s00586-010-1670-9.
Nygaard OP, Romner B, Trumpy JH. Duration of symptoms as a predictor of outcome after lumbar disc surgery. Acta Neurochir (Wien). 1994;128(1-4):53-56. doi: 10.1007/BF01400653.
Ng LC, Sell P. Predictive value of the duration of sciatica for lumbar discectomy. A prospective cohort study. J Bone Joint Surg Br. 2004;86(4):546-549. PMID: 15174551.
Omidi-Kashani F, Ghayem Hasankhani E, Kachooei AR, Rahimi MD, Khanzadeh R. Does duration of preoperative sciatica impact surgical outcomes in patients with lumbar disc herniation? Neurol Res Int. 2014;2014:565189. doi: 10.1155/2014/565189.
Kerr D, Zhao W, Lurie JD. What are long-term predictors of outcomes for lumbar disc herniation? A randomized and observational study. Clin Orthop Relat Res. 2015;473(6):1920-1930. doi: 10.1007/s11999-014-3803-7.
Atlas SJ, Keller RB, Wu YA, Deyo RA, Singer DE. Long-term outcomes of surgical and nonsurgical management of sciatica secondary to a lumbar disc herniation: 10 year results from the maine lumbar spine study. Spine (Phila Pa 1976). 2005;30(8):927-935. doi: 10.1097/01.brs.0000158954.68522.2a.
Mannion AF, Elfering A, Staerkle R, Junge A, Grob D, Semmer NK, et al. Outcome assessment in low back pain: how low can you go? Eur Spine J. 2005;14(10):1014-1026. doi: 10.1007/s00586-005-0911-9.
Peul WC, Arts MP, Brand R, Koes BW. Timing of surgery for sciatica: subgroup analysis alongside a randomized trial. Eur Spine J. 2009;18(4):538-545. doi: 10.1007/s00586-008-0867-7.
Mannion AF, Mutter UM, Fekete TF, Porchet F, Jeszenszky D, Kleinstück FS. Validity of a single-item measure to assess leg or back pain as the predominant symptom in patients with degenerative disorders of the lumbar spine. Eur Spine J. 2014;23(4):882-7. doi: 10.1007/s00586-014-3193-2.
Jönsson B, Annertz M, Sjöberg C, Strömqvist B. A prospective and consecutive study of surgically treated lumbar spinal stenosis. Part I: Clinical features related to radiographic findings. Spine (Phila Pa 1976). 1997;22(24):2932-2937. doi: 10.1097/00007632-199712150-00016.
Jönsson B, Annertz M, Sjöberg C, Strömqvist B. A prospective and consecutive study of surgically treated lumbar spinal stenosis. Part II: Five-year follow-up by an independent observer. Spine (Phila Pa 1976). 1997;22(24):2938-2944. doi: 10.1097/00007632-199712150-00017.
Blazhevski B, Filipche V, Cvetanovski V, Simonovska N. Predictive value of the duration of sciatica for lumbar discectomy. Prilozi. 2008;29(2):325-335. PMID: 19259056.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Al-Rafidain Journal of Medical Sciences ( ISSN 2789-3219 )

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Published by Al-Rafidain University College. This is an open access journal issued under the CC BY-NC-SA 4.0 license (https://creativecommons.org/licenses/by-nc-sa/4.0/).