Factors Contributing Towards COVID-19 Vaccination among Pregnant Women Attending Antenatal Clinics in a Tertiary Care Center, Bhubaneswar, India
DOI:
https://doi.org/10.54133/ajms.v5i.193الكلمات المفتاحية:
Antenatal women، COVID-19 vaccines، Pregnancy، Vaccine hesitancyالملخص
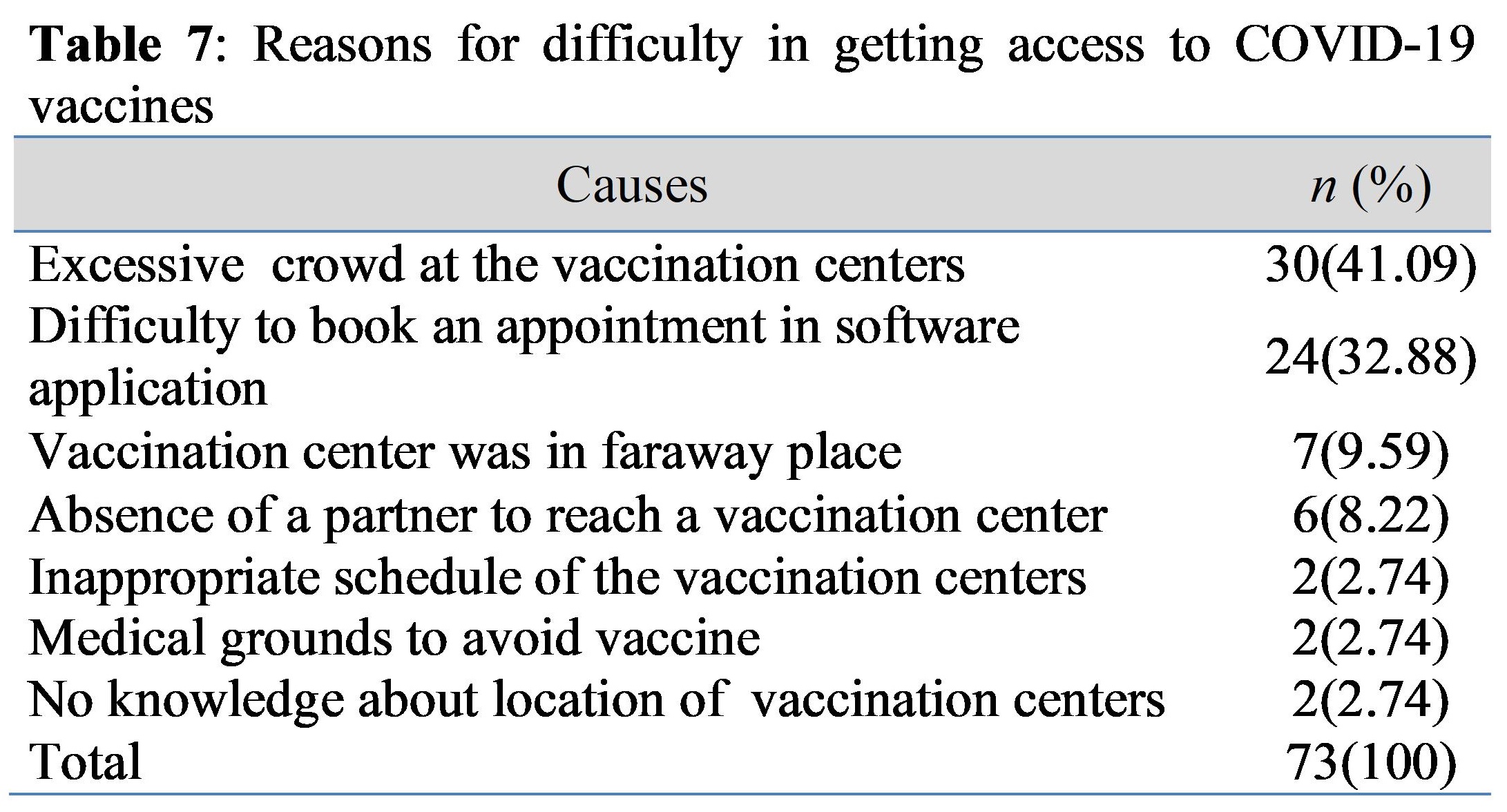
Background: Many vaccines were approved by the World Health Organization for emergency use in 2020, but pregnant women were excluded from these trials. When the COVID-19 vaccines were approved for use by pregnant women, they were left in a dilemma about whether to accept the vaccine during pregnancy or not. Objective: To study the factors contributing to COVID-19 vaccine hesitancy among pregnant women attending antenatal tertiary care centers in India. Method: A questionnaire was provided to pregnant women attending the antenatal tertiary care hospitals in Bhubaneswar, India. The questions included socio-demographic characteristics, obstetric parameters, knowledge of COVID-19 vaccines, and the reasons for hesitancy towards them. Results: Vaccine hesitancy was 29.34% among pregnant women. The sources of information regarding the vaccine were the internet, and the causes of vaccine hesitancy were inadequate information and mistrust of the vaccine. Younger women were more inclined to accept the vaccine. Primigravida, the second trimester of pregnancy, belonging to rural areas, and being homemakers were factors associated with hesitancy. Conclusions: Health care professionals need to actively participate in motivating pregnant women to accept the COVID-19 vaccines that should be integrated with the routine vaccination strategy in antenatal clinics.
التنزيلات
المراجع
Kuanar A, Kabi SK, Satapathy S, Mishra S, Bhuyan R, Kar D. Corona virus-A review concerns about the present scenario. Ann Rom Soc Cell Biol. 2021;25(2):1301-1315.
WHO: COVID-19 Vaccine Tracker and Landscape. 2021.
WHO issues its first emergency use validation for a COVID-19 vaccine and emphasizes need for equitable global access [Internet]. Available from: https://www.who.int/news/item/31-12-2020-who-issues-its-first-emergency-use-validation-for-a-covid-19-vaccine-and-emphasizes-need-for-equitable-global-access
Kumar VM, Pandi-Perumal SR, Trakht I, Thyagarajan SP. Strategy for COVID-19 vaccination in India: the country with the second highest population and number of cases. npj Vaccines. 2021;6(1). doi: 10.1038/s41541-021-00327-2. DOI: https://doi.org/10.1038/s41541-021-00327-2
Operational Guidance for COVID-19 Vaccination of Pregnant Women. Ministtry of Health and Family Welfare [Internet]. 2021;1-13. Available from: https://www.mohfw.gov.in/pdf/OperationalGuidanceforCOVID19vaccinationofPregnantWoman.pdf DOI: https://doi.org/10.4102/phcfm.v13i1.2998
Smith DD, Pippen JL, Adesomo AA, Rood KM, Landon MB, Costantine MM. Exclusion of pregnant women from clinical trials during the coronavirus disease 2019 pandemic: A review of international registries. Am J Perinatol. 2020;37(8):792-799. doi: doi: 10.1055/s-0040-1712103. DOI: https://doi.org/10.1055/s-0040-1712103
Goncu Ayhan S, Oluklu D, Atalay A, Menekse Beser D, Tanacan A, Moraloglu Tekin O, et al. COVID-19 vaccine acceptance in pregnant women. Int J Gynecol Obstet. 2021;154(2):291-296. doi: 10.1002/ijgo.13713. DOI: https://doi.org/10.1002/ijgo.13713
Riad A, Jouzová A, Üstün B, Lagová E, Hruban L, Janků P, et al. Covid-19 vaccine acceptance of pregnant and lactating women (Plw) in czechia: An analytical cross-sectional study. Int J Environ Res Public Health. 2021;18(24). doi: 10.3390/ijerph182413373. DOI: https://doi.org/10.3390/ijerph182413373
Skjefte M, Ngirbabul M, Akeju O, Escudero D, Hernandez-Diaz S, Wyszynski DF, et al. COVID-19 vaccine acceptance among pregnant women and mothers of young children: results of a survey in 16 countries. Eur J Epidemiol. 2021;36(2):197-211. doi: 10.1007/s10654-021-00728-6. DOI: https://doi.org/10.1007/s10654-021-00728-6
Allotey J, Stallings E, Bonet M, Yap M, Chatterjee S, Kew T, et al. Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease 2019 in pregnancy: Living systematic review and meta-analysis. BMJ. 2020;370. doi: 10.1136/bmj.m3320. DOI: https://doi.org/10.1136/bmj.m3320
Peepal P, Rath TS, Nayak S, Pendyala S. Maternal and neonatal outcomes among women with and without severe acute respiratory syndrome corona virus-2 infection: A retrospective analytical study. J Mother Child. 2021;25(2):77-85. doi: 10.34763/jmotherandchild.20212502.d-21-00021.
Dey M, Singh S, Tiwari R, Nair VG, Arora D, Tiwari S. Pregnancy outcome in first 50 sars-cov-2 positive patients at our center. Gynecol Obstet Reprod Med. 2021;27(1):1-6. doi: 10.21613/GORM.2021.1176. DOI: https://doi.org/10.21613/GORM.2021.1176
Tripathy GS, Rath TS, Behera S, Lekha KS, Kar D, Pendyala S. Effects of Covid-19 vaccination during pregnancy on the obstetric and neonatal outcomes in a tertiary health care center. J Mother Child. 2023;27(1):72-78. doi: 10.34763/jmotherandchild.20232701.d-22-00043.
Hinman AR. The eradication of Polio: Have we succeeded? Vaccine. 2017;35(42):5519-5521. doi: 10.1016/j.vaccine.2017.09.015. DOI: https://doi.org/10.1016/j.vaccine.2017.09.015
Durrheim DN, Crowcroft NS, Strebel PM. Measles - The epidemiology of elimination. Vaccine. 2014;32(51):6880-6883. doi: 10.1016/j.vaccine.2014.10.061. DOI: https://doi.org/10.1016/j.vaccine.2014.10.061
Hsu AL, Johnson T, Phillips L, Nelson TB. Sources of vaccine hesitancy: Pregnancy, infertility, minority concerns, and general skepticism. Open Forum Infect Dis. 2022;9(3):1-6. doi: 10.1093/ofid/ofab433. DOI: https://doi.org/10.1093/ofid/ofab433
Jarrett C, Wilson R, O’Leary M, Eckersberger E, Larson HJ, Eskola J, et al. Strategies for addressing vaccine hesitancy - A systematic review. Vaccine. 2015;33(34):4180-4190. doi: 10.1016/j.vaccine.2015.04.040. DOI: https://doi.org/10.1016/j.vaccine.2015.04.040
Benis A, Seidmann A, Ashkenazi S. Reasons for taking the COVID-19 vaccine by US social media users. Vaccines (Basel). 2021;9(4):1-17. doi: 10.3390/vaccines9040315. DOI: https://doi.org/10.3390/vaccines9040315
COVID-19 Vaccination Considerations for Obstetric–Gynecologic Care [Internet]. Available from: https://www.acog.org/clinical/clinical-guidance/practice-advisory/articles/2020/12/covid-19-vaccination-considerations-for-obstetric-gynecologic-care
Society for Maternal-Fetal Medicine. Society for Maternal-Fetal Medicine (SMFM) statement: SARS-CoV-2 vaccination in pregnancy [Internet]. Available from: https://s3.amazonaws.com/cdn.smfm.org/media/2591/SMFM_Vaccine_Statement_12-1-20_(final).pdf
Palamenghi L, Barello S, Boccia S, Graffigna G. Mistrust in biomedical research and vaccine hesitancy: the forefront challenge in the battle against COVID-19 in Italy. Eur J Epidemiol. 2020;35(8):785-788. doi: 10.1007/s10654-020-00675-8. DOI: https://doi.org/10.1007/s10654-020-00675-8
Gencer H, Özkan S, Vardar O. The effects of the COVID 19 pandemic on vaccine decisions in pregnant women. Women and Birth. 2020;35:317-323. doi: 10.1016/j.wombi.2021.05.003. DOI: https://doi.org/10.1016/j.wombi.2021.05.003
Robertson E, Reeve KS, Niedzwiedz CL, Moore J, Blake M, Green M, et al. Predictors of COVID-19 vaccine hesitancy in the UK household longitudinal study. Brain Behav Immun. 2021;94:41-50. doi: 10.1016/j.bbi.2021.03.008. DOI: https://doi.org/10.1016/j.bbi.2021.03.008
Weber J, Al-Tawfiq JA, Babcock HM, Bryant K, Drees M, Elshaboury R, et al. Multisociety statement on coronavirus disease 2019 (COVID-19) vaccination as a condition of employment for healthcare personnel. Infect Control Hosp Epidemiol. 2022;43(1):3-11. doi: 10.1017/ice.2021.322. DOI: https://doi.org/10.1017/ice.2021.322
Tao L, Wang R, Han N, Liu J, Yuan C, Deng L, et al. Acceptance of a COVID-19 vaccine and associated factors among pregnant women in China: a multi-center cross-sectional study based on health belief model. Hum Vaccines Immunother. 2021;17(8):2378-2388. doi: 10.1080/21645515.2021.1892432. DOI: https://doi.org/10.1080/21645515.2021.1892432
Hoque AM, Buckus S, Hoque M, Hoque ME, Van Hal G. COVID-19 Vaccine acceptability among pregnant women at a primary health care facility in Durban, South Africa. Eur J Med Heal Sci. 2020;2(5):1-6. doi: 10.24018/ejmed.2020.2.5.493. DOI: https://doi.org/10.24018/ejmed.2020.2.5.493
Kiefer MK, Mehl R, Costantine MM, Johnson A, Cohen J, Summerfield TL, et al. Characteristics and perceptions associated with COVID-19 vaccination hesitancy among pregnant and postpartum individuals: A cross-sectional study. BJOG An Int J Obstet Gynaecol. 2022;129(8):1342-1351. doi: 10.1111/1471-0528.17110. DOI: https://doi.org/10.1111/1471-0528.17110
Danchin MH, Costa-Pinto J, Attwell K, Willaby H, Wiley K, Hoq M, et al. Vaccine decision-making begins in pregnancy: Correlation between vaccine concerns, intentions and maternal vaccination with subsequent childhood vaccine uptake. Vaccine. 2018;36(44):6473-6479. doi: 10.1016/j.vaccine.2017.08.003. DOI: https://doi.org/10.1016/j.vaccine.2017.08.003
Blakeway H, Prasad S, Kalafat E, Heath PT, Ladhani SN, Le Doare K, et al. COVID-19 vaccination during pregnancy: coverage and safety. Am J Obstet Gynecol. 2022;226(2):236.e1-236.e14. doi: 10.1016/j.ajog.2021.08.007. DOI: https://doi.org/10.1016/j.ajog.2021.08.007
Anderson E, Brigden A, Davies A, Shepherd E, Ingram J. Maternal vaccines during the Covid-19 pandemic: A qualitative interview study with UK pregnant women. Midwifery. 2021;100:103062. doi: 10.1016/j.midw.2021.103062. DOI: https://doi.org/10.1016/j.midw.2021.103062
Januszek SM, Faryniak-Zuzak A, Barnaś E, Łoziński T, Góra T, Siwiec N, et al. The approach of pregnant women to vaccination based on a covid-19 systematic review. Medicine (Kaunas). 2021;57(9):1-11. doi: 10.3390/medicina57090977. DOI: https://doi.org/10.3390/medicina57090977
Sznajder KK, Kjerulff KH, Wang M, Hwang W, Ramirez SI, Gandhi CK. Covid-19 vaccine acceptance and associated factors among pregnant women in Pennsylvania 2020. Prev Med Rep. 2022;26:101713. doi: 10.1016/j.pmedr.2022.101713. DOI: https://doi.org/10.1016/j.pmedr.2022.101713
التنزيلات
منشور
كيفية الاقتباس
إصدار
القسم
الرخصة
الحقوق الفكرية (c) 2023 Al-Rafidain Journal of Medical Sciences

هذا العمل مرخص بموجب Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Published by Al-Rafidain University College. This is an open access journal issued under the CC BY-NC-SA 4.0 license (https://creativecommons.org/licenses/by-nc-sa/4.0/).