Maternal and Neonatal Outcomes of Gestational Thrombocytopenia in Pregnant Women from Kirkuk City, Iraq: A Case-Control Study
DOI:
https://doi.org/10.54133/ajms.v5i1S.324الكلمات المفتاحية:
Maternal outcomes، Neonatal outcomes، Pregnant women، Thrombocytopeniaالملخص
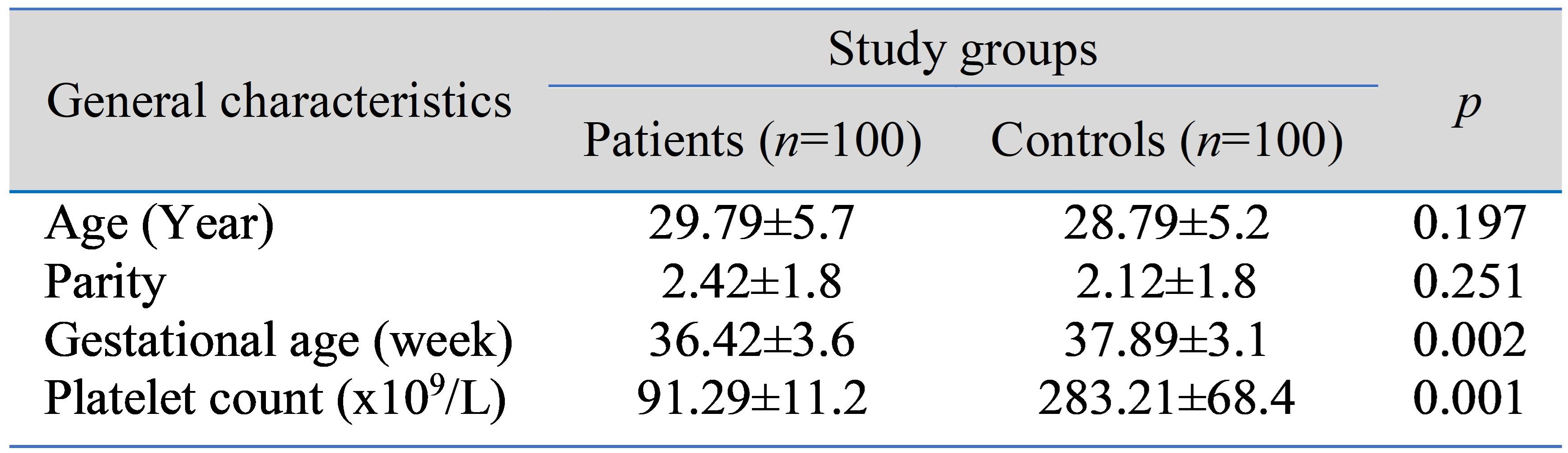
Background: Thrombocytopenia is the most common hematological disorder in pregnant women, second only to anemia. A platelet count of less than 150x109/L is regarded as low. It is the most common cause of thrombocytopenia during pregnancy when the platelet count does not fall below 70x109\L. Methods: A case-control study was carried out in the department of obstetrics and gynecology at Azadi Teaching Hospital, Kirkuk, Iraq. Two hundred pregnant women were enrolled in the study; they were divided into 100 cases and 100 controls. All participants were in labor at the time of admission. The cases were pregnant women with gestational thrombocytopenia, while the controls were pregnant women with a normal platelet count. A platelet count was performed for all participants using the Swelab Alfa Plus system. Results: mean gestational age and platelet count were significantly lower in patients than controls, while there was no statistically significant difference in age or parity between the study groups. Preterm labor, postpartum hemorrhage (PPH), intrauterine fetal growth restriction (IUGR), and intrapartum fetal distress were significantly higher in the patients than in the controls, and the mean APGAR score at 5 minutes was significantly lower in the patients compared to the controls. Conclusions: Pregnant women with gestational thrombocytopenia may be at higher risk of preterm labor, postpartum hemorrhage, IUGR, intrapartum fetal distress and a low neonatal APGAR score.
التنزيلات
المراجع
Ali Khalaf M, Khider DM, Kamal BJ. Anemia in pregnant women in Kirkuk Governorate. Kirkuk J Med Sci. 2020;8(1):78-85. doi: 10.32894/kjms.2020.169358.
McCrae KR. Thrombocytopenia in pregnancy. Hematology Am Soc Hematol Educ Program. 2010;2010(1):397-402. doi: 10.1182/asheducation-2010.1.397.
Park YH. Diagnosis and management of thrombocytopenia in pregnancy. Blood Res. 2022;57(S1):79-85. doi: 10.5045/br.2022.2022068.
Shehata N, Burrows R, Kelton JG. Gestational thrombocytopenia. Clin Obstet Gynecol. 1999;42(2):327-334. doi:10.1097/00003081-199906000-00017.
Jayawardena L, Mcnamara E. Diagnosis and management of pregnancies complicated by haemolysis, elevated liver enzymes and low platelets syndrome in the tertiary setting. Int Med J. 2020;50(3):342-349. doi: 10.1111/imj.14337.
Subtil SFC, Mendes JMB, Areia ALFA, Moura JPAS. Update on thrombocytopenia in pregnancy. Rev Bras Ginecol Obstet. 2020;42(12):834-840. doi: 10.1055/s-0040-1721350.
Burrows RF, Kelton JG. Fetal thrombocytopenia and its relation to maternal thrombocytopenia. N Engl J Med. 1993;329(20):1463-1466. doi:10.1056/NEJM199311113292005.
Perepu U, Rosenstein L. Maternal thrombocytopenia in pregnancy. Proc Obstet Gynecol. 2013;3(1): 1-15. Available from: http://ir.uiowa.edu/pog/
Reese JA, Peck JD, Deschamps DR, McIntosh JJ, Knudtson EJ, Terrell DR, et al. Platelet counts during pregnancy. N Engl J Med. 2018;379(1):32-43. doi:10.1056/NEJMoa1802897.
Mohammed EA. Postpartum maternal and neonatal outcomes of SARS-CoV-2 infection during pregnancy. Al-Rafidain J Med Sci. 2023;5: 67-72. doi: 10.54133/ajms.v5i.159
Nathan N, Sol I, Vincelot A, Collet D, Granchamp P, David E. Is a biological assessment necessary to realize an obstetrical epidural anaesthesia in a patient whose interrogation and clinical examination are strictly normal? Ann Fr Anesth Reanim. 2007;26(7-8):705-710. doi: 10.1016/j.annfar.2007.05.007.
Elveđi-Gašparović V, Beljan P, Gverić-Ahmetašević S, Schuster S, Škrablin S. Fetal-maternal complications and their association with gestational thrombocytopenia. Ginekol Pol. 2016;87(6):454-459. doi:10.5603/GP.2016.0025.
Kim BJ, Kim HS, Kim JH, Lee KY. Moderate to severe thrombocytopenia during pregnancy: A Single Institutional Experience. Indian J Hematol Blood Transfus. 2017;33(4):581-585. doi: 10.1007/s12288-017-0784-1.
Muhammad EM, Sabri EH, Saeed HD. The prevalence of thrombocytopenia in pregnant women in Baghdad: single centre study. J Fac Med Baghdad. 2018;60(2):98-101. doi: 10.32007/jfacmedbagdad.60213.
Gernsheimer T, James AH, Stasi R. How I treat thrombocytopenia in pregnancy. Blood. 2013;121(1):38-47. doi: 10.1182/blood-2012-08-448944.
Cines DB, Levine LD. Thrombocytopenia in pregnancy. Hematology Am Soc Hematol Educ Program. 2017;2017(1):144-151. doi: 10.1182/asheducation-2017.1.144.
Habas ES, Rayani A, Alfitori G, Eldin Ahmed G, Elzouki AY. Gestational thrombocytopenia: A Review on recent updates. Cureus. 2022;14(3):e23204. doi: 10.7759/cureus.23204.
Borhany M, Abid M, Zafar S, Zaidi U, Munzir S, Shamsi T. Thrombocytopenia in pregnancy: Identification and management at a reference center in Pakistan. Cureus. 2022;14(3). doi: 10.7759/cureus.23490.
Yousif A. The significance of asymptomatic gestational thrombocytopenia. Med J Tikrit University. 2017;22(1):96-102.
Zutshi V, Gupta N, Arora R, Dhanker S. Prevalence of gestational thrombocytopenia and its effect on maternal and fetal outcome. Iraqi J Hematol. 2019;8:21-24. doi: 10.4103/ijh.ijh_17_18.
Taş B, Günenc O. Maternal and fetal outcomes of gestational thrombocytopenia. Duzce Med J. 2022; 24(3): 282-286. doi: 10.18678/dtfd.1162645.
Nagey DA, Alger LS, Edelman BB, Heyman MR, Pupkin MJ, Crenshaw C. Reacting appropriately to thrombocytopenia in pregnancy. South Med J. 1986;79(11):1385-1388. doi: 10.1097/00007611-198611000-00017.
Ciobanu AM, Colibaba S, Cimpoca B, Peltecu G, Panaitescu AM. Thrombocytopenia in pregnancy. Maedica (Bucur). 2016;11(1):55-60. PMID: 28465752.
التنزيلات
منشور
كيفية الاقتباس
إصدار
القسم
الرخصة
الحقوق الفكرية (c) 2023 Al-Rafidain Journal of Medical Sciences

هذا العمل مرخص بموجب Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Published by Al-Rafidain University College. This is an open access journal issued under the CC BY-NC-SA 4.0 license (https://creativecommons.org/licenses/by-nc-sa/4.0/).