DOI:
https://doi.org/10.54133/ajms.v6i1.437الكلمات المفتاحية:
DOAC، Medication adherence، Self-efficacy، Warfarinالملخص
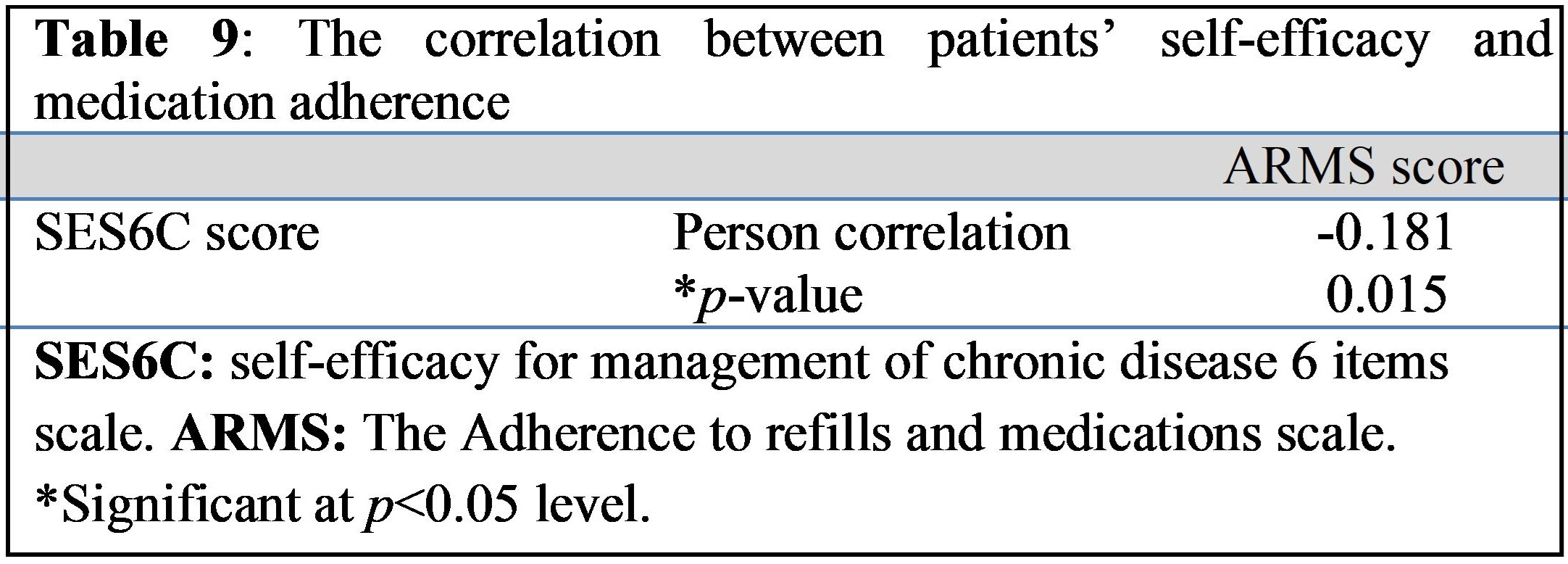
Background: While warfarin and direct oral anticoagulants (DOACs) are used to manage thromboembolic events, they possess several features that impact adherence. Objective: To assess medication adherence and self-efficacy in patients receiving warfarin or DOAC treatment. Methods: A cross-sectional study was performed at Ibn Al-Bitar Hospital in Baghdad from December 2022 to May 2023 on patients receiving either warfarin or DOACs. The Arabic version of the Adherence to Refills and Medications Scale (ARMS) questionnaire and the Self-Efficacy for Managing Chronic Disease 6-Item Scale (SES6C) questionnaire were used to assess adherence and self-efficacy. Results: 181 patients were enrolled in the study, of whom 56.9% received warfarin and 43.1% received DOACs. The mean ARMS score was 13.71, and 81.77% of the patients were adherent to anticoagulant therapy. There was a significant difference in adherence between the warfarin and DOAC groups. The mean SES6C score for the participants was 50.01. Patients in the DOAC group had significantly higher self-efficacy compared to those in the warfarin group. The adherence score correlated significantly with patients’ gender, education level, hospitalization and duration of anticoagulant use, while the SES6C score did not correlate with any of the independent variables. There was a significant negative correlation between self-efficacy scores and medication adherence scores. Conclusions: Patients receiving DOACs showed a higher self-efficacy to manage chronic diseases and lower medication adherence as compared to warfarin. Higher self-efficacy was associated with higher adherence to treatment.
التنزيلات
المراجع
Weitz JI, Harenberg J. New developments in anticoagulants: Past, present and future. Thrombosis and Haemostasis. 2017;117(07):1283–1288. doi: 10.1160/TH16-10-0807.
Holbrook AM, Pereira JA, Labiris R, et al. Systematic overview of warfarin and its drug and food interactions. Arch Intern Med. 2005;165(10):1095-1106. doi: 10.1001/archinte.165.10.1095.
Wadelius M, Chen LY, Eriksson N, Bumpstead S, Ghori J, Wadelius C, et al. Association of warfarin dose with genes involved in its action and metabolism. Hum Genetics. 2007;121(1):23–34. doi: 10.1007/s00439-006-0260-8.
Baglin T. Clinical use of new oral anticoagulant drugs: dabigatran and rivaroxaban. Br J Hematol. 2013;163(2):160–167. doi: 10.1111/ bjh.12502.
Czuprynska J, Patel JP, Arya R. Current challenges and future prospects in oral anticoagulant therapy. Br J Haematol. 2017;178(6):838–851. doi: 10.1111/bjh.14714.
De Caterina R, Prisco D, Eikelboom JW. Factor XI inhibitors: cardiovascular perspectives. Eur Heart J. 2023;44(4):280–292. doi: 10.1093/eurheartj/ehac464.
Organization WHO (2003) Adherence to long-term therapies: evidence for action. p 211. https://www.who.int/chp/knowledge/publications/adherence_full_report.pdf?ua=1
Raparelli V, Proietti M, Cangemi R, Lip GY, Lane DA, Basili S. Adherence to oral anticoagulant therapy in patients with atrial fibrillation. Focus on non-vitamin K antagonist oral anticoagulants. Thromb Haemost. 2017;117(2):209-218. doi: 10.1160/TH16-10-0757.
Giner-Soriano M, Sotorra Figuerola G, Cortés J, Pera Pujadas H, Garcia-Sangenis A, Morros R. Impact of medication adherence on mortality and cardiovascular morbidity: Protocol for a population-based cohort study. JMIR Res Protocols. 2018;7(3):e73. doi: 10.2196/resprot.8121.
Bonsu KO, Young SW, Lee T, Nguyen HV, Chitsike RS. Self-reported adherence to direct oral anticoagulants versus warfarin therapy in a specialized thrombosis service-a cross-sectional study of patients in a Canadian Health Region. Eur J Clin Pharmacol. 2023;79(1):117–125. doi: 10.1007/s00228-022-03418-8.
Bandura A, Freeman WH, Lightsey R. Self-Efficacy: The exercise of control. J Cogn Psychother. 1997;13(2):158–166.
Brady TJ, Murphy L, O’Colmain BJ, Beauchesne D, Daniels B, Greenberg M, et al. A meta-analysis of health status, health behaviors, and health care utilization outcomes of the chronic disease self-management program. Prevent Chronic Dis. 2013;10:120112. doi: 10.5888/pcd10.120112.
Huang YM, Shiyanbola O, Smith P. Association of health literacy and medication self-efficacy with medication adherence and diabetes control. Patient Prefer Adhere. 2018; 12:793–802. doi: 10.2147/PPA.S153312.
Al-Jabi SW, Dalu AA, Koni AA, Khdour MR, Taha AA, Amer R, et al. The relationship between self-efficacy and treatment satisfaction among patients with anticoagulant therapy: a cross-sectional study from a developing country. Thrombosis J. 2022;20(1):15. doi: 10.1186/s12959-022-00374-2.
Alalaqi A, Lawson G, Obaid Y, Tanna S. Adherence to cardiovascular pharmacotherapy by patients in Iraq: A mixed methods assessment using quantitative dried blood spot analysis and the 8-item Morisky Medication Adherence Scale. Thakur SS, editor. Plos One. 2021;16(5):e0251115. doi: 10.1371/journal.pone.0251115.
Al-Ganmi AHA, Alotaibi A, Gholizadeh L, Perry L. Medication adherence and predictive factors in patients with cardiovascular disease: A cross-sectional study. Nurs Health Sci. 2020;22(2):454-463. doi: 10.1111/nhs.12681.
Ghayadh AA, Naji AB. Treatment adherence and its association to quality of life among patients with hypertension. Pakistan Heart J. 2023;56(2):44–49.
Raheem Z, Mohammed TR. Evaluation of patients’ knowledge and adherence to clopidogrel therapy post percutaneous coronary intervention. Iraqi Nat J Nurs Specialt. 2023;36(1):117–124.
Fadhil O, Gorial FI. Medications adherence among sample of patients with ankylosing spondylitis. Iraqi Postgrad Med J. 2023;22(1):33-40.
Al-Tuma Ali, Jassim NA. Adherence to methotrexate in Iraqi patients with rheumatoid arthritis: A cross-sectional study. Glob J Public Health Med. 2022;4(1):618-630. doi: 10.37557/gjphm.v4i1.146.
Mikhael EM. Assessing the adherence to insulin therapy and the effect of injection pain on insulin adherence among type 2 diabetes mellitus patients. J Pharm Negative Results. 2020;11(1):65–68.
Showaya AH, Jawad KA. Correlation between adherence to medication and social support on patients with diabetes mellitus. Pakistan Heart J. 2023;56(2):696–698.
Jabbar RK, Jammal MY. Factors associated with adherence to insulin self-administration among children and adolescents with type 1 DM in Iraq. Iraqi J Pharm Sci. 2023;32(Suppl.):291–999. doi: 10.31351/vol32issSuppl.pp291-299.
Madran DM, Jassim AH. Self-efficacy and its relationship to self-care among type II diabetic patients. Int J Health Sci. 2022;6(S2):15199–15208. doi: 10.53730/ijhs.v6nS2.8851.
Hamza SH, Faraj RK. Self-efficacy for clients with diabetes mellitus type II who attend to diabetic center in Al-Diwaniyah city. Indian J Forens Med Toxicol. 2021;15(3):5372–5379. doi: 10.37506/ijfmt.v15i3.16284.
Alammari G, Alhazzani H, AlRajhi N, Sales I, Jamal A, Almigbal TH, et al. Validation of an Arabic version of the adherence to refills and medications scale (ARMS). Healthcare. 2021;9(11):1430. doi: 10.3390/healthcare9111430.
Kripalani S, Risser J, Gatti ME, Jacobson TA. Development and evaluation of the Adherence to Refills and Medications Scale (ARMS) among low-literacy patients with chronic disease. Value Health. 2009;12(1):118-123. doi: 10.1111/j.1524-4733.2008.00400.x.
Allam MM, El-Zawawy HT, Ibrahim Ismail I, Ghazy RM. Cross-cultural reliability of an Arabic version of the self-efficacy for managing chronic disease 6-item scale in Arab patients with diabetes mellitus. Prim Care Diabetes. 2020;14(4):305-310. doi: 10.1016/j.pcd.2019.11.001.
Lorig KR, Sobel DS, Ritter PL, Laurent D, Hobbs M. Effect of a self-management program on patients with chronic disease. Effective Clin Pract. 2001;4(6):256–262.
Chen PT, Wang TJ, Hsieh MH, Liu JC, Liu CY, Wang KY, et al. Anticoagulation adherence and its associated factors in patients with atrial fibrillation: a cross-sectional study. BMJ Open. 2019;9(9):e029974. doi: 10.1136/bmjopen-2019-029974.
Miyazaki M, Nakashima A, Nakamura Y, Sakamoto Y, Matsuo K, Goto M, et al. Association between medication adherence and illness perceptions in atrial fibrillation patients treated with direct oral anticoagulants: An observational cross-sectional pilot study. PloS One. 2018;13(9):e0204814. doi: 10.1371/journal.pone.0204814.
Yao X, Abraham NS, Alexander GC, Crown W, Montori VM, Sangaralingham LR, et al. Effect of adherence to oral anticoagulants on risk of stroke and major bleeding among patients with atrial fibrillation. J Am Heart Assoc. 2016;5(2):e003074. doi: 10.1161/JAHA.115.003074.
Patel SI, Cherington C, Scherber R, Barr K, McLemore R, Morisky DE, et al. Assessment of patient adherence to direct oral anticoagulant vs. warfarin therapy. J Am Osteopathic Assoc. 2017;117(1):7-15. doi: 10.7556/jaoa.2017.002.
Obamiro KO, Chalmers L, Lee K, Bereznicki BJ, Bereznicki LR. Adherence to Oral Anticoagulants in Atrial Fibrillation: An Australian Survey. J Cardiovasc Pharmacol Ther. 2018;23(4):337–343. doi: 10.1177/1074248418770201.
Caspard H, Chan AK, Walker AM. Compliance with a statin treatment in a usual-care setting:Retrospective database analysis over 3 years after treatment initiation in health maintenance organization enrollees with dyslipidemia. Clin Ther. 2005;27(10):1639–1646. doi: 10.1016/j.clinthera.2005.10.005.
Mayet AY. Patient adherence to warfarin therapy and its impact on anticoagulation control. Saudi Pharm J. 2016;24(1):29–34. doi: 10.1016/j.jsps.2015.02.005.
Mobini S, Allahbakhshian A, Shabanloei R, Sarbakhsh P. Illness perception, self-efficacy, and medication adherence in patients with coronary artery disease: A path analysis of conceptual model. SAGE Open Nurs. 2023;9:1-14. doi: 10.1177/23779608231171772.
Uchmanowicz B, Chudiak A, Uchmanowicz I, Rosińczuk J, Froelicher ES. Factors influencing adherence to treatment in older adults with hypertension. Clin Interven Aging. 2018;13:2425–2441. doi: 10.2147/CIA.S182881.
Lai YF, Neo JK, Cheen MH, Kong MC, Tai BC, Ng HJ. Comparison of medication adherence and treatment persistence between new oral anticoagulant and warfarin among patients. Ann Acad Med Singapore. 2016;45(1):12–17.
Nemer O, Malak MZ. Self-efficacy and self-care behaviors among patients with coronary artery disease in Jordan. Int Res J Pharm Med Sci. 2022;5(2):32-47.
Shen Z, Shi S, Ding S, Zhong Z. Mediating effect of self-efficacy on the relationship between medication literacy and medication adherence among patients with hypertension. Front Pharmacol. 2020;11:569092. doi: 10.3389/fphar.2020.569092.
Lestari ND, Anisa VN. The relationship between self efficacy and medication adherence in elderly with hypertension. Bali Med J. 2022;11(3):1660–1665.
D’Souza MS, Al Salmi NMD. Self-efficacy impact adherence in diabetes mellitus. Diabetes Updates. 2018;4(6). doi: 10.15761/DU.1000111.
التنزيلات
منشور
كيفية الاقتباس
إصدار
القسم
الرخصة
الحقوق الفكرية (c) 2024 Al-Rafidain Journal of Medical Sciences

هذا العمل مرخص بموجب Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Published by Al-Rafidain University College. This is an open access journal issued under the CC BY-NC-SA 4.0 license (https://creativecommons.org/licenses/by-nc-sa/4.0/).