The Effect of Systemic Proteolytic Enzymes on Postoperative Inflammatory Response and Quality of Life after Surgical Extraction of Impacted Mandibular Third Molar
DOI:
https://doi.org/10.54133/ajms.v7i1.848الكلمات المفتاحية:
Bromelain، Health care، Pain، Quality of life، Third molar، Tibrolinالملخص
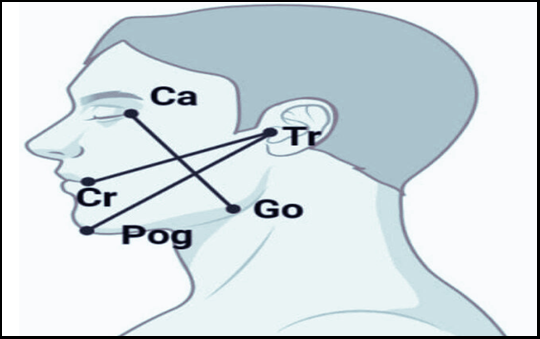
Background: The surgical extraction of impacted third molar usually results in postoperative inflammation manifested as pain, facial swelling and trismus which may cause deterioration in the patient’s quality of life. Methods: This randomized controlled study included 56 patients indicated for surgical extraction of IMTM under local anesthesia. These patients were randomly assigned into two groups: a study group that included patients who received Tibrolin® postoperatively and a control group that did not. The predictor variable was whether to use SET or not. Pain measured by the pain numerical rating scale (NRS), facial swelling, and the degree of trismus were the outcome variables. The Arabic version of the Oral Health Impact Profile 5 (OHIP5-Ar) questionnaire was used to measure quality of life (QoL) on the day of surgery (day 1) and on days 3, 7, and 13. Results: The study group demonstrated significantly lower pain scores postoperatively on day 1 and a lesser degree of facial swelling on day 3 compared to the control group, while no significant differences were observed regarding the other time intervals. There were no significant differences in the degree of trismus or QoL between the two groups. Conclusions: Tibrolin® administration following the surgical extraction of IMTM might reduce post-operative complaints in patients with surgical extraction of IMTM.
التنزيلات
المراجع
Lateef TA, Bede SYH, Mohammed JA. The influence of prophylactic Dexamethasone on postoperative swelling and trismus following impacted mandibular third molar surgical extraction. J Bagh Coll Dent. 2010;22(4):85-90.
Bede SY. Factors affecting the duration of surgical extraction of impacted mandibular third molars. World J Dent. 2018;9(1):8–12. doi: 10.5005/jp-journals-10015-1498. DOI: https://doi.org/10.5005/jp-journals-10015-1498
Veronez B, Matos FP de, Monnazzi MS, Sverzut AT, Sverzut CE, Trivellato AE. Maxillofacial infection. A retrospective evaluation of eight years. Brazilian J Oral Sci. 2014;2(13):98–103. doi: 10.1590/1677-3225v13n2a04. DOI: https://doi.org/10.1590/1677-3225v13n2a04
Shabat MA, Bede SY. Effect of the local application of bupivacaine in early pain control following impacted mandibular third molar surgery: A randomized controlled study. Dent Med Probl. 2021;58(4):483–488. doi: 10.17219/dmp/133664. DOI: https://doi.org/10.17219/dmp/133664
Kareem ASA, Al Hussaini AH. Effect of platelet rich-fibrin on alveolar osteitis incidence following surgical removal of impacted mandibular third molars: A comparative study. J Bagh Coll Dent. 2019;31(4):63-70.doi:10.26477//jbcd.v31i4.2723. DOI: https://doi.org/10.26477/jbcd.v31i4.2723
O’Sullivan L, Ríordáin RN. Variations in reporting of clinician-reported outcome measures in third molar surgery: A focused review. Surg. 2022;20(3):43–50. doi: 10.1016/j.surge.2021.03.008. DOI: https://doi.org/10.1016/j.surge.2021.03.008
Shin YS. How to improve the national health insurance fee-for-service schedule? Health Welfare Forum. 2019;20(6):39–52.
Lago-Méndez L, Diniz-Freitas M, Senra-Rivera C, Gude-Sampedro F, Gándara Rey JM, García-García A. Relationships between surgical difficulty and postoperative pain in lower third molar extractions. J Oral Maxillofac Surg. 2007;65(5):979-983. doi: 10.1016/j.joms.2006.06.281. DOI: https://doi.org/10.1016/j.joms.2006.06.281
Jerjes W, El-Maaytah M, Swinson B, Upile T, Thompson G, Gittelmon S, et al. Inferior alveolar nerve injury and surgical difficulty prediction in third molar surgery: the role of dental panoramic tomography. J Clin Dent. 2006;17(5):122-130. PMID: 17240930.
Contar CM, de Oliveira P, Kanegusuku K, Berticelli RD, Azevedo-Alanis LR, Machado MA. Complications in third molar removal: a retrospective study of 588 patients. Med Oral Patol Oral Cir Bucal. 2010;15(1):e74-78. doi: 10.4317/medoral.15.e74. DOI: https://doi.org/10.4317/medoral.15.e74
Abhinandan U, Arvind R, Srikant N. Comparison of anti-inflammatory efficacy of three different therapeutic modalities after mandibular third molar impaction surgery-a cross sectional study. J Int Dent Med Res. 2022;15(4):1684–1689.
Gandhewar T, Andrade NN, Aggarwal N, Choradia S, Mathai PC, Nerurkar S. The effects of systemic proteolytic enzyme therapy on pain and swelling in third molar surgery equal to diclofenac therapy: a prospective randomized double blinded clinical trial. Oral Maxillofac Surg. 2020;24(4):461-468. doi: 10.1007/s10006-020-00854-7. DOI: https://doi.org/10.1007/s10006-020-00854-7
Yuan G, Wahlqvist ML, He G, Yang M, Li D. Natural products and anti-inflammatory activity. Asia Pac J Clin Nutr. 2006;15(2):143-152. PMID: 16672197.
Maurer HH, Tauvel FX, Kraemer T. Screening procedure for detection of non-steroidal anti-inflammatory drugs and their metabolites in urine as part of a systematic toxicological analysis procedure for acidic drugs and poisons by gas chromatography-mass spectrometry after extractive methyl. J Anal Toxicol. 2001;25(4):237–244. doi: 10.1093/jat/25.4.237. PMID: 11386636. DOI: https://doi.org/10.1093/jat/25.4.237
Inchingolo F, Tatullo M, Marrelli M, Inchingolo AM, Picciariello V, Inchingolo AD, et al. Clinical trial with bromelain in third molar exodontia. Eur Rev Med Pharmacol Sci. 2010;14(9):771–774. PMID: 21061836.
Majid OW, Al-Mashhadani BA. Perioperative bromelain reduces pain and swelling and improves quality of life measures after mandibular third molar surgery: a randomized, double-blind, placebo-controlled clinical trial. J Oral Maxillofac Surg. 2014;72(6):1043–1048. doi: 10.1016/j.joms.2013.12.035. DOI: https://doi.org/10.1016/j.joms.2013.12.035
Mameli A, Natoli V, Casu C. Bromelain: An Overview of Applications in Medicine and Dentistry. Biointerface Res Appl Chem. 2020;11(1):8165–8170.doi: 10.33263/BRIAC111.81658170. DOI: https://doi.org/10.33263/BRIAC111.81658170
Kaur R, Abmwani S, Mehta B. Trypsin, rutoside and bromelain alone and fixed dose combination: a natural, safer and effective anti-inflammatory agent. J Drug Deliv Ther. 2014;4(1):108–110. DOI: https://doi.org/10.22270/jddt.v4i1.746
A, Langade D, Sonawane D, Gavai P. A randomized, clinical trial to evaluate efficacy and tolerability of trypsin: chymotrypsin as compared to serratiopeptidase and trypsin: bromelain: rutoside in wound management. Adv Ther. 2017;34(1):180–198. doi: 10.1007/s12325-016-0444-0. DOI: https://doi.org/10.1007/s12325-016-0444-0
Mendes ML, do Nascimento-Júnior EM, Reinheimer DM, Martins-Filho PR. Efficacy of proteolytic enzyme bromelain on health outcomes after third molar surgery. Systematic review and meta-analysis of randomized clinical trials. Med Oral Patol Oral Cir Bucal. 2019;24(1):e61-e69. doi: 10.4317/medoral.22731. DOI: https://doi.org/10.4317/medoral.22731
Kwatra B. A review on potential properties and therapeutic applications of bromelain. World J Pharm Pharm Sci. 2019;8(11):488–500. doi: 10.20959/wjpps201911-14941.
Kumar ST, Prasanna RA, Kirubanandan JR, Elaveyini U, Devi SP, Balasubramaniam M. Postoperative healing after surgical removal of mandibular third molar: A comparative study between two proteolytic enzymes. J Pharm Bioallied Sci. 2020;12(1):289-294. doi: 10.4103/jpbs.JPBS_87_20. DOI: https://doi.org/10.4103/jpbs.JPBS_87_20
Wala LJ. Clinical evaluation of anti-Inflammatory properties of combination of bromelain trypsin and rutoside with combination of ibuprofen trypsin and chymotrypsin following third molar extraction–A comparative study. Rajiv Gandhi Univ Health Sci (India). 2017;8(2):468-468.
Vishal KT, Priya S, Sinha DK, Kumar C. Effect of bromelain, rutoside and trypsin combination on postoperative pain, swelling and trismus after surgical third Mmolar extraction. J West Bengal Univ Heal Sci. 2021;1(3):18–25.
Abhinav RP. Systemic enzymes and their role in the reduction of post-operative edema after surgical removal of lower third molars: A randomized controlled double-blind study. J Popul Ther Clin Pharmacol. 2023;30(6):200–206. doi: 10.47750/jptcp.2023.30.06.027. DOI: https://doi.org/10.47750/jptcp.2023.30.06.027
Thorat SD, Nilesh K. Efficacy of low-level laser therapy in the management of postoperative surgical sequelae after surgical removal of impacted mandibular third molars. Natl J Maxillofac Surg. 2022;13(1):52-56. doi: 10.4103/njms.NJMS_52_20. DOI: https://doi.org/10.4103/njms.NJMS_52_20
Wala LJ, Choudhary A, Reddy BC. Clinical evaluation of anti-inflammatory properties of combination of bromelain, trypsin and rutoside with combination of ibuprofen, trypsin and chymotrypsin following third molar extraction–A comparative study. J Med Sci Clin Res. 2020;8(2):464-468. DOI: https://doi.org/10.18535/jmscr/v8i2.81
Liu S, Zhao H, Wang Y, Zhao H, Ma C. Oral bromelain for the control of facial swelling, trismus, and pain after mandibular third molar surgery: a systematic review and meta-analysis. J Oral Maxillofac Surg. 2019;77(8):1566-1574. doi: 10.1016/j.joms.2019.02.044. DOI: https://doi.org/10.1016/j.joms.2019.02.044
Sato FRL, Asprino L, de Araújo DES, de Moraes M. Short-term outcome of postoperative patient recovery perception after surgical removal of third molars. J Oral Maxillofac Surg. 2009;67(5):1083–1091. doi: 10.1016/j.joms.2008.09.032. DOI: https://doi.org/10.1016/j.joms.2008.09.032
De la Barrera-Núñez MC, Yáñ ez-Vico RM, Batista-Cruzado A, Heurtebise-Saavedra JM, Castillo-de Oyagüe R, Torres-Lagares D. Prospective double-blind clinical trial evaluating the effectiveness of Bromelain in the third molar extraction postoperative period. Med Oral Patol Oral Cir Bucal. 2014;19(2):157-162. doi: 10.4317/medoral.19105. DOI: https://doi.org/10.4317/medoral.19105
Daftary GV, Shah AP, Divekar GH, John J, Patil NN. Systemic therapy with bromelain-trypsin-rutoside combination in inflammation: A narrative review of the pharmacodynamics. Natl J Physiol Pharm Pharmacol. 2022;12(10):1521-1528. doi: 10.5445/njpp.2022.12.1037420212502202. DOI: https://doi.org/10.5455/njppp.2022.12.10374202125022022
De Marco G, Lanza A, Cristache CM, Capcha EB, Espinoza KI, Rullo R, et al. The influence of flap design on patients’ experiencing pain, swelling, and trismus after mandibular third molar surgery: a scoping systematic review. J Appl Oral Sci. 2021;29:e20200932. doi: 10.1590/1678-7757-2020-0932. DOI: https://doi.org/10.1590/1678-7757-2020-0932
Villela GA, Mariano RC, de Menezes PHM, Saraiva MCP, Antoniali C. Does etoricoxib or Ddexamethasone control inflammatory pain, edema, and trismus after impacted third molar surgery? A double-blind, split-mouth randomized clinical trial. J Anesth Clin Res. 2023;14:1106. doi: 10.35248/2155-6148.23.14.1106. DOI: https://doi.org/10.21203/rs.3.rs-2675608/v1
Majid OW. Submucosal dexamethasone injection improves quality of life measures after third molar surgery: a comparative study. J Oral Maxillofac Surg. 2011;69(9):2289–2297. doi: 10.1016/j.joms.2011.01.037. DOI: https://doi.org/10.1016/j.joms.2011.01.037
Alhajj MN, Halboub E, Khalifa N, Amran AG, Reissmann DR, Abdullah AG, et al. Translation and validation of the Arabic version of the 5-item Oral health impact profile: OHIP5-Ar. Health Qual Life Outcomes. 2018;16:218. doi: 10.1186/s12955-018-1046-0. DOI: https://doi.org/10.1186/s12955-018-1046-0
McGrath C, Comfort MB, Lo ECM, Luo Y. Changes in life quality following third molar surgery–the immediate postoperative period. Br Dent J. 2003;194(5):265–268. doi: 10.1038/sj.bdj.4809930. DOI: https://doi.org/10.1038/sj.bdj.4809930
Savin J, Ogden GR. Third molar surgery—a preliminary report on aspects affecting quality of life in the early postoperative period. Br J Oral Maxillofac Surg. 1997;35(4):246–253. doi: 10.1016/s0266-4356(97)90042-5. DOI: https://doi.org/10.1016/S0266-4356(97)90042-5
التنزيلات
منشور
كيفية الاقتباس
إصدار
القسم
الرخصة
الحقوق الفكرية (c) 2024 Al-Rafidain Journal of Medical Sciences

هذا العمل مرخص بموجب Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Published by Al-Rafidain University College. This is an open access journal issued under the CC BY-NC-SA 4.0 license (https://creativecommons.org/licenses/by-nc-sa/4.0/).