Effects of Lycopene as Monotherapy or Combined with Clobetasol on Spleen Index and Inflammatory Markers in Mouse Model of Imiquimod-Induced Psoriasis
DOI:
https://doi.org/10.54133/ajms.v4i.118Keywords:
Lycopene, Psoriasis, Imiquimod-induced psoriasis, Mice, SpleenAbstract
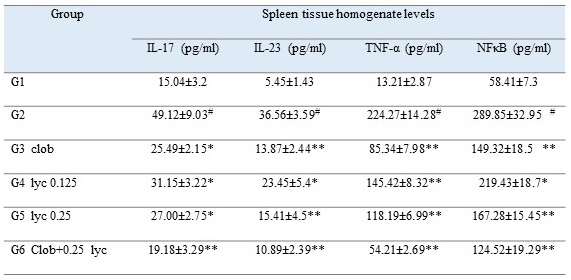
Background: Lycopene has demonstrated favorable impacts on diverse health conditions, particularly those of an inflammatory nature. Objective: To evaluate the impact of topical application of lycopene on the spleens of mice with psoriasis induced by imiquimod (IMQ). Methods: The study employed a sample size of 48 mice, divided into six groups of eight mice each. The experimental protocol involved the application of IMQ to each of the five groups twice. The first application was administered for six days to induce psoriasis, followed by a second application for another six days while the tested medications were concurrently administered, with the exception of the first group, which served as the control group. Following the six-day induction phase, group 2 was treated exclusively with petrolatum jelly. On the other hand, groups 3-6 were subjected to different treatments, including clobetasol propionate, lycopene at concentrations of 0.125 mg/ml and 0.25 mg/ml, and a combination of 0.05% clobetasol and 0.25 mg/ml of lycopene. Each of the examined pharmaceutical substances was administered topically once daily for a duration of six days at the IMQ application site. Results: Lycopene at a concentration of 0.25 mg/ml resulted in a significant reduction in the spleen index and a restoration of the tissue levels of inflammatory mediators (TNF-α, IL-23, NF-κB, and IL-17) that were close to normal. Conclusion: The anti-inflammatory properties of lycopene can significantly aid in the normalization of spleens in patients who have developed psoriasis due to imiquimod.matory capabilities.
Downloads
References
Nestle FO, Kaplan DH, Barker J. Psoriasis. N Engl J Med. 2009;361(5):496-509. doi: 10.1056/NEJMra0804595. DOI: https://doi.org/10.1056/NEJMra0804595
Prinz JC. The role of T cells in psoriasis. J Eur Acad Dermatol Venereol. 2003;17(3):257-270. doi: 10.1046/j.1468-3083.2003.00720.x. DOI: https://doi.org/10.1046/j.1468-3083.2003.00720.x
Pariser D, Schenkel B, Carter C, Farahi K, Brown TM, Ellis CN; Psoriasis Patient Interview Study Group. A multicenter, non-interventional study to evaluate patient-reported experiences of living with psoriasis. J Dermatol Treat. 2016;27(1):19-26. doi: 10.3109/09546634.2015.1044492. DOI: https://doi.org/10.3109/09546634.2015.1044492
Griffiths CE, Barker JN. Pathogenesis and clinical features of psoriasis. Lancet. 2007;370(9583):263-271. doi: 10.1016/S0140-6736(07)61128-3. DOI: https://doi.org/10.1016/S0140-6736(07)61128-3
Bachelez H, van de Kerkhof PC, Strohal R, Kubanov A, Valenzuela F, Lee JH, et al. Tofacitinib versus etanercept or placebo in moderate-to-severe chronic plaque psoriasis: a phase 3 randomized non-inferiority trial. Lancet. 2015;386(9993):552-561. doi: 10.1016/S0140-6736(14)62113-9. DOI: https://doi.org/10.1016/S0140-6736(14)62113-9
Bogen S, Pak J, Garifallou M, Deng X, Muller WA. Monoclonal antibody to murine PECAM-1 (CD31) blocks acute inflammation in vivo. J Exp Med. 1994;179:1059-1064. doi: 10.1084/jem.179.3.1059. DOI: https://doi.org/10.1084/jem.179.3.1059
Byamba D, Kim DY, Kim DS, Kim TG, Jee H, Kim SH, et al. Skin-penetrating methotrexate alleviates imiquimod-induced psoriasiform dermatitis via decreasing IL-17-producing gamma delta T cells. Exp Dermatol. 2014;23(7):492-496. doi: 10.1111/exd.12448. DOI: https://doi.org/10.1111/exd.12448
Hwang ES, Lee HJ. Inhibitory effects of lycopene on the adhesion, invasion, and migration of SK-Hep1 human hepatoma cells. Exp Biol Med. 2006;231(3):322-327. doi: 10.1177/153537020623100313. DOI: https://doi.org/10.1177/153537020623100313
Gajendragadkar PR, Hubsch A, Mäki-Petäjä KM, Serg M, Wilkinson IB, Cheriyan J. Effects of oral lycopene supplementation on vascular function in patients with cardiovascular disease and healthy volunteers: a randomized controlled trial. PLoS One. 2014;9(6):e99070. doi: 10.1371/journal.pone.0099070. DOI: https://doi.org/10.1371/journal.pone.0099070
Kim JY, Paik JK, Kim OY, Park HW, Lee JH, Jang Y, et al. Effects of lycopene supplementation on oxidative stress and markers of endothelial function in healthy men. Atherosclerosis. 2011;215(1):189-195. doi: 10.1016/j.atherosclerosis.2010.11.036. DOI: https://doi.org/10.1016/j.atherosclerosis.2010.11.036
Yang PM, Chen HZ, Huang YT, Hsieh CW, Wung BS. Lycopene inhibits NF-κB activation and adhesion molecule expression through Nrf2-mediated heme oxygenase-1 in endothelial cells. Int J Mol Med. 2017;39(6):1533-1450. doi: 10.3892/ijmm.2017.2960. DOI: https://doi.org/10.3892/ijmm.2017.2960
Chen P, Xu S, Qu J. Lycopene protects keratinocytes against UVB radiation-induced carcinogenesis via negative regulation of FOXO3a through the mTORC2/AKT signaling pathway. J Cell Biochem. 2018;119(1):366-377. doi: 10.1002/jcb.26189. DOI: https://doi.org/10.1002/jcb.26189
Allen LV, Ansel HC. Ansel's pharmaceutical dosage forms and drug delivery systems (10th edition), Wolters Kluwer Health Business; 2014; Page 237
Sun J, Zhao Y, Hu J. Curcumin inhibits imiquimod-induced psoriasis-like inflammation by inhibiting IL-1beta and IL-6 production in mice. PLoS One. 2013;8(6):e67078. doi: 10.1371/journal.pone.0067078. DOI: https://doi.org/10.1371/journal.pone.0067078
Shih CM, Hsieh CK, Huang CY, Huang CY, Wang KH, Fong TH, et al. Lycopene inhibit IMQ-induced psoriasis-like inflammation by inhibiting ICAM-1 production in mice. Polymers (Basel). 2020;12(7):1521. doi: 10.3390/polym12071521. DOI: https://doi.org/10.3390/polym12071521
Parasuraman S, Raveendran R, Kesavan R. Blood sample collection in small laboratory animals. J Pharmacol Pharmacother. 2010;1(2):87-93. doi: 10.4103/0976-500X.72350. DOI: https://doi.org/10.4103/0976-500X.72350
Arora N, Shah K, Pandey-Rai S. Inhibition of imiquimod-induced psoriasis-like dermatitis in mice by herbal extracts from some Indian medicinal plants. Protoplasma. 2016;253(2):503-515. doi: 10.1007/s00709-015-0829-y. DOI: https://doi.org/10.1007/s00709-015-0829-y
Harper EG, Guo C, Rizzo H, Lillis JV, Kurtz SE, Skorcheva I, et al. Th17 cytokines stimulate CCL20 expression in keratinocytes in vitro and in vivo: implications for psoriasis pathogenesis. J Invest Dermatol. 2009;129(9):2175-2183. doi: 10.1038/jid.2009.65. DOI: https://doi.org/10.1038/jid.2009.65
Caldarola G, De Simone C, Carbone A, Tulli A, Amerio P, Feliciani C. TNFalpha and its receptors in psoriatic skin, before and after treatment with etanercept. Int J Immunopathol Pharmacol. 2009;22(4):961-966. doi: 10.1177/039463200902200411. DOI: https://doi.org/10.1177/039463200902200411
Bugaut H, Aractingi S. Major role of the IL17/23 axis in psoriasis supports the development of new targeted therapies. Front Immunol. 2021;12:621956. doi: 10.3389/fimmu.2021.621956. DOI: https://doi.org/10.3389/fimmu.2021.621956
Abdou AG, Hanout HM. Evaluation of survivin and NF-kappaB in psoriasis, an immunohistochemical study. J Cutan Pathol. 2008;35(5):445-451. doi: 10.1111/j.1600-0560.2007.00841.x. DOI: https://doi.org/10.1111/j.1600-0560.2007.00841.x
Janet PL, Philip PJ, (Eds.), Oxford handbook of medical statistics, (Ch 8), Oxford University Press, UK, 2011; pp 237.
Sun L, Yu G, Jiang H, Shi K, Huang D, Bao H, et al. Experimental study on the anti-inflammatory effect of Mongolian medicine sendeng decoction on mice with psoriasis. Med Novel Technol Devices. 2022;16:100154. doi: 10.1016/j.medntd.2022.10015. DOI: https://doi.org/10.1016/j.medntd.2022.100154
Chen H, Lu C, Liu H, Wang M, Zhao H, Yan Y, et al. Quercetin ameliorates imiquimod-induced psoriasis-like skin inflammation in mice via the NF-κB pathway. Int Immunopharmacol. 2017;48:110-117. doi: 10.1016/j.intimp.2017.04.022. DOI: https://doi.org/10.1016/j.intimp.2017.04.022
Na Takuathung M, Wongnoppavich A, Panthong A, Khonsung P, Chiranthanut N, Soonthornchareonnon N, et al. Antipsoriatic effects of Wannachawee recipe on imiquimod-induced psoriasis-like dermatitis in BALB/c mice. Evid Based Complement Alternat Med. 2018;2018:7931031. doi: 10.1155/2018/7931031. DOI: https://doi.org/10.1155/2018/7931031
Redegeld FA, Yu Y, Kumari S, Charles N, Blank U. Non-IgE mediated mast cell activation. Immunol Rev. 2018;282(1):87-113. doi: 10.1111/imr.12629. DOI: https://doi.org/10.1111/imr.12629
Zeichner JA, Armstrong A. The role of IL-17 in the pathogenesis and treatment of psoriasis. J Clin Aesthet Dermatol. 2016;9(6 Suppl 1):S3-S6. PMID: 28439340.
Armstrong AW, Mehta MD, Schupp CW, Gondo GC, Bell SJ, Griffiths CEM. Psoriasis Prevalence in adults in the United States. JAMA Dermatol. 2021;157(8):940-946. doi: 10.1001/jamadermatol.2021.2007. DOI: https://doi.org/10.1001/jamadermatol.2021.2007
Takahashi H, Tsuji H, Honma M, Ishida-Yamamoto A, Iizuka H. Increased plasma resistin and decreased omentin levels in Japanese patients with psoriasis. Arch Dermatol Res. 2013;305(2):113-116. doi: 10.1007/s00403-012-1310-9. DOI: https://doi.org/10.1007/s00403-012-1310-9
van de Kerkhof PC. An update on topical therapies for mild-moderate psoriasis. Dermatol Clin. 2015;33(1):73-77. doi: 10.1016/j.det.2014.09.006. DOI: https://doi.org/10.1016/j.det.2014.09.006
Adcock IM, Lane SJ. Corticosteroid-insensitive asthma: molecular mechanisms. J Endocrinol. 2003;178(3):347-355. doi: 10.1677/joe.0.1780347. DOI: https://doi.org/10.1677/joe.0.1780347
Sarkar S. A treatise on topical corticosteroid in dermatology. Indian J Dermatol. 2018;63(6):530-531. doi: 10.4103/ijd.IJD_297_18.
Schoepe S, Schäcke H, May E, Asadullah K. Glucocorticoid therapy-induced skin atrophy. Exp Dermatol. 2006;15(6):406-420. doi: 10.1111/j.0906-6705.2006.00435.x. DOI: https://doi.org/10.1111/j.0906-6705.2006.00435.x
Krinsky NI, Johnson EJ. Carotenoid actions and their relation to health and disease. Mol Aspects Med. 2005;26(6):459-516. doi: 10.1016/j.mam.2005.10.001. DOI: https://doi.org/10.1016/j.mam.2005.10.001
Fazekas Z, Gao D, Saladi RN, Lu Y, Lebwohl M, Wei H. Protective effects of lycopene against ultraviolet B-induced photodamage. Nutr Cancer. 2003;47(2):181-187. doi: 10.1207/s15327914nc4702_11. DOI: https://doi.org/10.1207/s15327914nc4702_11
Hiragun M, Hiragun T, Oseto I, Uchida K, Yanase Y, Tanaka A, Okame T, Ishikawa S, Mihara S, Hide M, et al. Oral administration of β-carotene or lycopene prevents atopic dermatitis-like dermatitis in HR-1 mice. J Dermatol. 2016;43(10):1188-1192. doi: 10.1111/1346-8138.13350. DOI: https://doi.org/10.1111/1346-8138.13350
Hugh JM, Weinberg JM. Update on the pathophysiology of psoriasis. Cutis. 2018;102(5S):6-12. PMID: 30566550.
Sun S, Cao C, Li J, Meng Q, Cheng B, Shi B, et al. Lycopene modulates placental health and fetal development under high-fat diet during pregnancy of rats. Mol Nutr Food Res. 2021;65(14):e2001148. doi: 10.1002/mnfr.202001148. DOI: https://doi.org/10.1002/mnfr.202001148
Elmets CA, Korman NJ, Prater EF, Wong EB, Rupani RN, Kivelevitch D, et al. Joint AAD-NPF Guidelines of care for the management and treatment of psoriasis with topical therapy and alternative medicine modalities for psoriasis severity measures. J Am Acad Dermatol. 2021;84(2):432-470. doi: 10.1016/j.jaad.2020.07.087. DOI: https://doi.org/10.1016/j.jaad.2020.07.087
Mohammed SS, Kadhim HM, Al-Sudani IM, Musatafa WW. Study the topical effect of six days use of different lycopene doses on imiquimod-induce psoriasis-like skin inflammation in mice. Int J Health Sci. 2022;6(S3):171-185. doi: 10.53730/ijhs.v6nS3.5241. DOI: https://doi.org/10.53730/ijhs.v6nS3.5241
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Al-Rafidain Journal of Medical Sciences ( ISSN: 2789-3219 )

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Published by Al-Rafidain University College. This is an open access journal issued under the CC BY-NC-SA 4.0 license (https://creativecommons.org/licenses/by-nc-sa/4.0/).