Association between Albuminuria, Glycated Hemoglobin with Comorbidities in Type 2 Diabetes Patients: Experience in Sulaimani City, Iraq
DOI:
https://doi.org/10.54133/ajms.v6i1.380الكلمات المفتاحية:
Albuminuria، Comorbidities، HBA1c، Sulaimani City، Type 2 diabetes mellitusالملخص
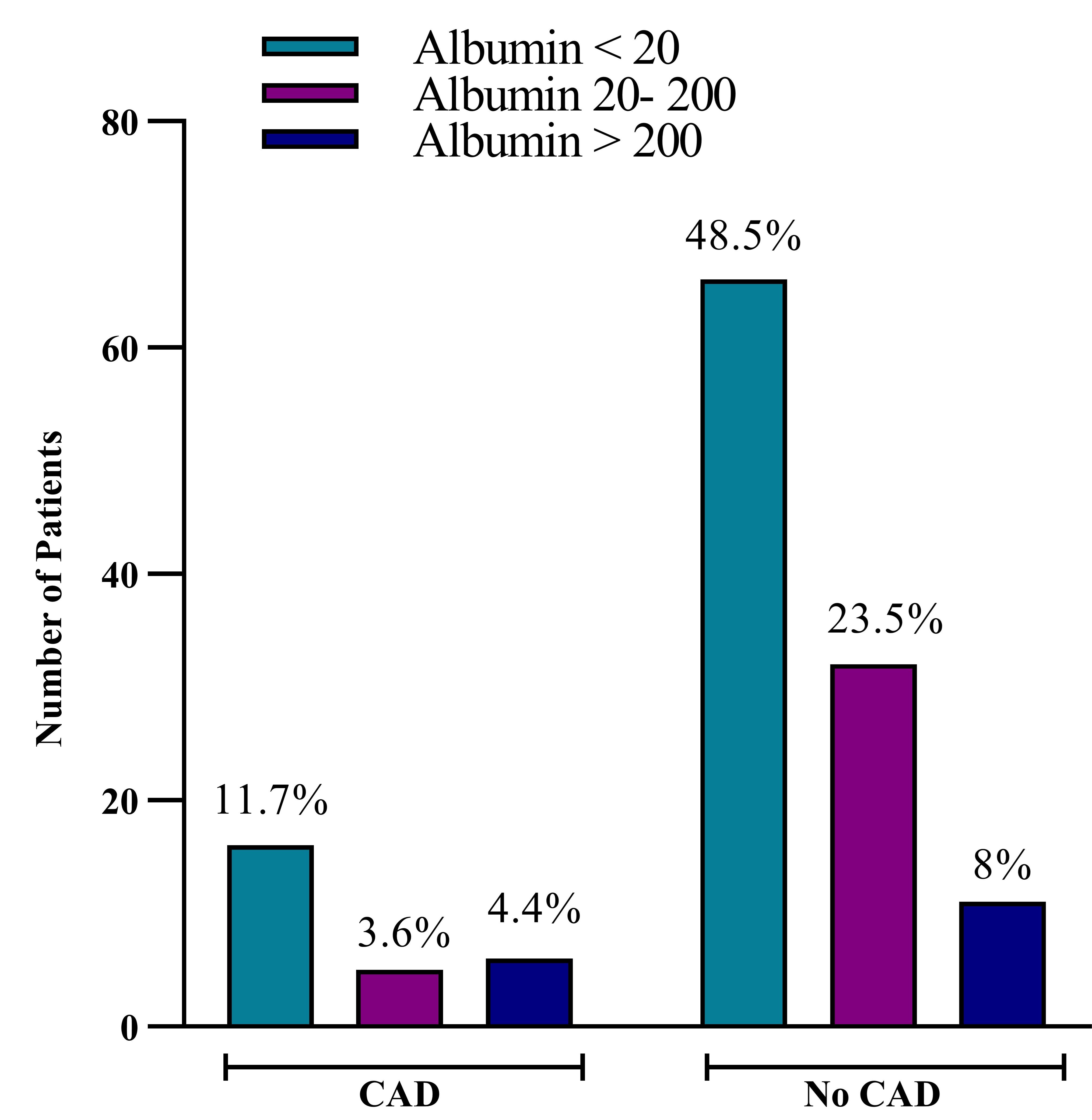
Background: Diabetes nephropathy is one of the most important complications of type 2 diabetes mellitus (T2DM). Albuminuria is an early clinical indicator for investigating diabetes nephropathy. Age, poor glycemic control, long duration of diabetes, and hypertension increase the risk of albuminuria. Objectives: To determine the relationship between albuminuria, HbA1c, and comorbidities in elderly patients with T2DM. Methods: A cross-sectional study was carried out on 136 elderly patients with T2DM at the Diabetes and Endocrine Center in Sulaimani City. Data was obtained from each patient through face-to-face interviews and laboratory tests for HbA1c, serum lipid profiles, and albumin levels in the urine. Results: Out of 136 patients, 82 elderly patients with T2DM were normoalbuminuric, 37 had microalbuminuria, and 17 had macroalbuminuria, respectively. The female gender was at greater risk of developing albuminuria (19.1% microalbuminuria and 6.6% macroalbuminuria) than the male gender (8% microalbuminuria and 5.8% macroalbuminuria). The risk factors for microalbuminuria and macroalbuminuria were poor glycemic control (HBA1c >7.5) (16.9% microalbuminuria and 6.6% macroalbuminuria), long-term diabetes (5–10 years) (13.9% microalbuminuria and 5.1% macroalbuminuria), and coexisting comorbidity conditions (21.3%) microalbuminuria and 10.2% macroalbuminuria, mainly hypertension (20.5% microalbuminuria and 8.8% macroalbuminuria). Conclusion: Our findings showed that the incidence of albuminuria in elderly patients with T2DM was high in patients with poor diabetes control, a long duration of diabetes, and comorbidity conditions, particularly in patients with hypertension.
التنزيلات
المراجع
Upamali S, Rathnayake S. Perspectives of older people with uncontrolled type 2 diabetes mellitus towards medication adherence: A qualitative study. Plos one. 2023;18(8):1-18. doi: 10.1371/journal.pone.0289834.
Mansoori A, Sahranavard T, Hosseini ZS, Soflaei SS, Emrani N, Nazar E, et al. Prediction of type 2 diabetes mellitus using hematological factors based on machine learning, 17 approaches: a cohort study analysis. Sci Rep. 2023;13(1):1-11. doi: 10.1038/s41598-022-27340-2.
Papatheodorou K, Banach M, Bekiari E, Rizzo M, Edmonds M. Complications of diabetes 2017. J Diabetes Res. 2018;2018:1-4. doi: 10.1155/2018/3086167 .
Ramanathan RS. Correlation of duration, hypertension and glycemic control with microvascular complications of diabetes mellitus at a tertiary care hospital. J Neurol Exp Neural Sci. 2017;4(1):1-4. doi: 10.29011/JNNS-120.100020.
Ighodaro OM, Adeosun AM. Vascular complications in diabetes mellitus. Glob J Endocrinol Metab. 2017;1(2):1-3. doi: 10.31031/GJEM.2017.01.000506.
Ohiagu FO, Chikezie PC, Chikezie CM. Pathophysiology of diabetes mellitus complications: Metabolic events and control. Biomed Res Ther. 2021;8(3):4243-57. doi: 10.15419/bmrat.v8i3.663.
Maranta F, Cianfanelli L, Cianflone D. Glycaemic control and vascular complications in diabetes mellitus type 2. Adv Exp Med Biol. 2021;1307:129-152 doi: 10.1007/5584_2020_514.
Hu Q, Chen Y, Deng X, Li Y, Ma X, Zeng J, et al. Diabetic nephropathy: Focusing on pathological signals, clinical treatment, and dietary regulation. Biomed Pharmacother. 2023;159:1-16. doi: 10.1016/j.biopha.2023.114252.
Mohammed O, Alemayehu E, Bisetegn H, Debash H, Gedefie A, Ebrahim H, et al. Prevalence of microalbuminuria among diabetes patients in Africa: A systematic review and meta-analysis. Diabetes Metab Syndr Obes. 2023;16:2089-2103. doi: 10.2147/DMSO.S409483.
Karimifar M, Afsar J, Amini M, Moeinzadeh F, Feizi A, Aminorroaya A. The effect of linagliptin on microalbuminuria in patients with diabetic nephropathy: a randomized, double blinded clinical trial. Sci Rep. 2023;13(1):1-9. doi: 10.1038/s41598-023-30643-7.
Harahap RI, Tristina N, Anriani RR. Comparations of glycated albumin among type 2 diabetes mellitus patient with normoalbuminuria, microalbuminuria and macroalbuminuria. J Med Sci. 2023;17(1):53-58. doi: 10.26891/JIK.v17i1.2023.
Wang Y, Yuan A, Yu C. Correlation between microalbuminuria and cardiovascular events. Int J Clin Exp Med. 2013;6(10):973-978. PMCID: PMC3832337.
Rask-Madsen C, King GL. Vascular complications of diabetes: mechanisms of injury and protective factors. Cell Metab. 2013;17(1):20-33. doi: 10.1016/j.cmet.2012.11.012.
Chowdhury SK, Datta S, Mohith MT, Roy S, Hossain MJ, Zafrin N, et al. Study of relationship between HbA1c and microalbuminuria of diabetic patients. Ann Intern Med Dent Res. 2022;8(2):99-108. doi: 10.53339/aimdr.2022.8.2.14.
Martínez MM, Causillo TC, Agüero JE, Silva MG. Microalbuminuria as a marker of kidney damage in patients with diabetes mellitus. J Clin Med Rev. 2022;1(1):2836-2330. doi: 10.58489/2836-2330/001.
Jatoi NA, Said AH, Al-Ghamdi MS, Al-Abdulmhsin MF, Bin-Jaban RA, Al-Tayeb JA, et al. Prevalence of microalbuminuria and cardiovascular risk factors in patients with diabetes mellitus type-II in Al-Khobar, Kingdom of Saudi Arabia. Cureus. 2022;14(10):1-8. doi: 10.7759/cureus.29808.
Bhattarai T, Pandey A, Parajuli S, Khanal P, Dongol A, Devkota R, et al. Microalbuminuria among patients with diabetes mellitus visiting the department of nephrology in a tertiary care centre: A descriptive cross-sectional study. J Nepal Med Assoc. 2023;61(263):596-598. doi: 10.31729/jnma.8214.
Hu H, Zhao X, Jin X, Wang S, Liang W, Cong X. Efficacy and safety of eplerenone treatment for patients with diabetic nephropathy: a meta-analysis. PLoS One. 2022;17(3):1-16. doi: 10.1371/journal.pone.0265642.
Kim YJ, Hwang SW, Lee T, Lee JY, Uh Y. Association between urinary albumin creatinine ratio and cardiovascular disease. PLoS One. 2023;18(3):1-12. doi: 10.1371/journal.pone.0283083.
Ghimire P, Upadhyay HP. Albuminuria in patients with type 2 diabetes mellitus: a single center cross-sectional study. J Coll Med Sci Nepal. 2022;18(2):144-152. doi: 10.3126/jcmsn.v18i2.46099.
Khan TM, Nawaz FK, Karim MS, Shafique Z, Anwar MS, Usman O. Incidence of microalbuminuria and factors affecting it in patients with type 2 diabetes mellitus. Cureus. 2022;14(7):1-6. doi: 10.7759/cureus.27294.
Belli BG. Microalbuminuria in patients with type 2 Diabetes mellitus and its correlation with dyslipidemia. RGUHS J Med Sci. 2020;10(1):35-41. doi:10.26463/rjms.10_1_8.
Hussein NA. The prevalence of micro albuminuria in type 2 diabetes mellitus patients. Med J Babylon. 2014;11(4):984-93.
Lambers Heerspink HJ, Brantsma AH, de Zeeuw D, Bakker SJ, de Jong PE, et al. Albuminuria assessed from first-morning-void urine samples versus 24-hour urine collections as a predictor of cardiovascular morbidity and mortality. Am J Epidemiol. 2008;168(8):897-905. doi: 10.1093/aje/kwn209.
Iqbal A, Salman J, Habib J, Ali M, Naveed S, Ali A. Frequency of microalbuminuria and its relation to HbA1C in type 2 Diabetes mellitus patients. Professional Med J. 2023;30(02):199-203. doi: 10.29309/TPMJ/2023.30.02.6972.
Shikata K, Kodera R, Utsunomiya K, Koya D, Nishimura R, Miyamoto S, et al. Prevalence of albuminuria and renal dysfunction, and related clinical factors in Japanese patients with diabetes: The Japan Diabetes Complication and its Prevention prospective study 5. J Diabetes Investig. 2020;11(2):325-332. doi: 10.1111/jdi.13116.
Sana MA, Chaudhry M, Malik A, Iqbal N, Zakiuddin A, Abdullah M. Prevalence of microalbuminuria in type 2 diabetes mellitus. Cureus. 2020;12(12):1-4. doi: 10.7759/cureus.12318.
Al-Futaisi A, Al-Zakwani I, Almahrezi A, Al-Hajri R, Al-Hashmi L, Al-Muniri A, et al. Prevalence and predictors of microalbuminuria in patients with type 2 diabetes mellitus: a cross-sectional observational study in Oman. Diabetes Res Clin Pract. 2006;72(2):212-215. doi: 10.1016/j.diabres.2005.10.001.
Abdelwahid HA, Dahlan HM, Mojemamy GM, Darraj GH. Predictors of microalbuminuria and its relationship with glycemic control among type 2 diabetic patients of Jazan Armed Forces Hospital, southwestern Saudi Arabia. BMC Endocr Disord. 2022;22(1):1-8. doi: 10.1186/s12902-022-01232-y.
Al-Shammak AA, Ali AD, Jermozy HA. Prevalence of proteinuria among type 2 diabetic patients in Dhamar Governorate, Yemen. Int J Diabetes Clin Res. 2019;6(2):1-7. doi: 10.23937/2377-3634/1410106.
Tandon RK, Khare A, Gupta M, Nandwani S, Bansal R, Sharma S. Relationship between glycosylated hemoglobin and risk of microalbuminuria in patients with type 2 diabetes mellitus. People’s J Sci Res. 2015;8(1):14-18.
Al-Maskari F, El-Sadig M, Obineche E. Prevalence and determinants of microalbuminuria among diabetic patients in the United Arab Emirates. BMC Nephrol. 2008;9:1. doi: 10.1186/1471-2369-9-1.
Bae ES, Hur JY, Jang HS, Kim JS, Kang HS. Risk factors of microalbuminuria among patients with type 2 diabetes mellitus in Korea: A cross-sectional study based on 2019–2020 Korea National Health and Nutrition Examination Survey Data. Int J Environ Res Public Health. 2023;20(5):1-11. doi: 10.3390/ijerph20054169.
Aleidan AM, Al-Hamad E, Aleidan AM. Prevalence and gender difference in microalbuminuria among diabetic patients attending primary healthcare center at Security Forces Hospital, Riyadh, Saudi Arabia. Ann Clin Anal Med. 2023;10(1):232-239. doi: 10.4328/acam.v10i1.2.
Ali AA, Al Lami FH. Prevalence and determinants of microalbuminurea among type 2 diabetes mellitus patients, Baghdad, Iraq, 2013. Saudi J Kidney Dis Transpl. 2016;27(2):348-355. doi: 10.4103/1319-2442.178561.
Afkhami-Ardekani M, Modarresi M, Amirchaghmaghi E. Prevalence of microalbuminuria and its risk factors in type 2 diabetic patients. Indian J Nephrol. 2008;18(3):112-117. doi: 10.4103/0971-4065.43690.
Bamahel AS. Prevalence of diabetic nephropathy among type 2 diabetes mellitus patients in Mukalla City, Yemen. Enhanced Knowl Sci Technol. 2022;2(2):432-440. doi: doi: 10.30880/ekst.2022.02.02.046.
Nakhjavani M, Morteza A, Jenab Y, Ghaneei A, Esteghamati A, Karimi M, et al. Gender difference in albuminuria and ischemic heart disease in type 2 diabetes. Clin Med Res. 2012;10(2):51-56. doi: 10.3121/cmr.2011.1021.
Das SK, Patjoshi SK, Narayan CB, Nayak DR, Yadav RN. Assessment among type 2 diabetes mellitus relationship with albuminuria. Int J Acad Med Pharm. 2023;5(4):911-915. doi: 10.47009/jamp.2023.5.4.184.
Atalla AA, Abdullah AM, Turkistani AK, Aljawi MA, Al-Habashi AH. The prevalence and risk factors of micro and macroalbuminuria among diabetic patients in Taif. Mid East J Fam Med. 2022;21(1):299-303. doi: 10.5742/MEWFM.2023.95251599.
Lin YP. Albuminuria in hypertension. Hypertens Res. 2013;36(9):762-764. doi: 10.1038/hr.2013.76.
Li F, Chen QX, Peng B, Chen Y, Yao T, Wang G. Microalbuminuria in patients with acute ischemic stroke. Neurol Res. 2019;41(6):498-503. doi: 10.1080/01616412.2019.1576320.
Makino H, Haneda M, Babazono T, Moriya T, Ito S, Iwamoto Y, et al. Microalbuminuria reduction with telmisartan in normotensive and hypertensive Japanese patients with type 2 diabetes: a post-hoc analysis of The Incipient to Overt: Angiotensin II Blocker, Telmisartan, Investigation on Type 2 Diabetic Nephropathy (INNOVATION) study. Hypertens Res. 2008;31(4):657-664. doi: 10.1291/hypres.31.657.
التنزيلات
منشور
كيفية الاقتباس
إصدار
القسم
الرخصة
الحقوق الفكرية (c) 2024 Al-Rafidain Journal of Medical Sciences

هذا العمل مرخص بموجب Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Published by Al-Rafidain University College. This is an open access journal issued under the CC BY-NC-SA 4.0 license (https://creativecommons.org/licenses/by-nc-sa/4.0/).